"Mood Disorder Expert to Speak at Williams"
iBerkshires.com - March 26, 2008
WILLIAMSTOWN — One of the world's foremost authorities on mood disorders, Kay Redfield Jamison, will speak on "Personal and Professional Perspectives on Mental Illness" at Williams College on Wednesday, April 9.
The event will take place at 7:30 p.m. in Chapin Hall.
Jamison is professor of psychiatry at Johns Hopkins Medical School and co-director of the Johns Hopkins Mood Disorders Center. She is the co-author of the standard medical text on manic-depressive illness, which was chosen as the Most Outstanding Book in Biomedical Sciences by the American Association of Publishers in 1990.
She is also author of "An Unquiet Mind," her memoir about her experiences with manic-depressive illness. "An Unquiet Mind" was on The New York Times best seller list for more than five months and translated into 20 languages.
Jamison is the recipient of the National Mental Health Association's William Styron Award, the American Suicide Foundation Research Award, the Community Mental Health Leadership Award, and was a 2001 MacArthur Fellowship recipient.
Formerly the director of the UCLA Affective Disorders Clinic, she has been cited as one of the "Best Doctors in the United States." She has been awarded numerous honorary degrees, selected as one of five individuals for the public television series "Great Minds of Medicine," and chosen by Time magazine as a "Hero of Medicine."
Her other publications include "Exuberance: The Passion for Life" and "Night Falls Fast: Understanding Suicide." "Touched with Fire: Manic- Depressive Illness and the Artistic Temperament" is one of Jamison's most intriguing publications. She investigates the lives of artists like Van Gogh, Byron, and Virginia Woolf to suggest that most prominent artists are manic-depressives and investigate the connection between the illness and genius.
Jamison received her doctorate in psychology from the University of California at Los Angeles. She also studied zoology and neurophysiology at the University of St. Andrews in Scotland.
Free and open to the public, this lecture is the culminating event of the three-day program "Mental Health Matters: Reducing Stress, Distress, and Stigma at Williams" and is sponsored by Psychological Counseling Services, the Lecture Committee and the chaplain's office, with a number of other Williams organizations.
For more information contact John.A.Miner@williams.edu or mwood@williams.edu.
www.iberkshires.com/story/26552/Mood-Disorder-Expert-to-Speak-at-Williams.html
"Mental Health Matters: Reducing Stress, Distress, and STIGMA at Williams"
--
Reader's Comments:
President Shapiro:
I am sorely disappointed that Williams confers a "stigma" upon mental health matters. It is my understanding that the ADA specifically prohibits higher education from so doing, that we are entitled to a discrimination free education.
Richard.L.Nesbitt: Can you assure me students would not be subjected to a "stigma" there, as this program states?
Harold A. Maio
Advisory Board
American Journal of Psychiatric Rehabilitation
Board Member
Partners in Crisis
Former Consulting Editor
Psychiatric Rehabilitation Journal
Boston University
Language Consultant
UPENN Collaborative on Community Integration
of Individuals with Psychiatric Disabilities
Home:
8955 Forest St
Ft Myers FL 33907
239-275-5798
khmaio@earthlink.net
from: on: 03-26-2008
--
----------
"Support name change for DMR"
The Berkshire Eagle - Letters
Saturday, May 03, 2008
What's in a name? For people served by the Massachusetts Department of Mental Retardation and their families and friends, this is a very important question. The label "mental retardation" is part of a classification system for people who score below 70-75 on an IQ test. In the past, this classification was qualified by additional labels including the terms of moron, imbecile, and idiot. All of these labels are derogatory and highly offensive to people with and without developmental disabilities.
Derogatory language is disrespectful language. Massachusetts is one of only five states that continues to use the term "mental retardation" to identify a public human service department.
In an incredible response to this advocacy, our legislators have developed legislation — House Bill 4610 — that is currently before the Ways and Means Committee. As it stands, this legislation supports a change of the name of the department to the "Massachusetts Department of Developmental Disabilities Services." This name change misses the mark. The board would like the name changed to the "Massachusetts Department of Developmental Services." This name eliminates the term "disability" that is deficit-focused and derogatory, and more accurately describes the people and services that the department is intended to support. This was the proposed name change by the original sponsor of the bill, prior to it being amended in committee.
The board joins with people served by the department to urge the citizens of our state to change the name of the Massachusetts Department of Mental Retardation to the "Massachusetts Department of Developmental Services." To make this change, we need citizens of our state to contact their legislators to request their action on House Bill 4610 and to amend this bill to change the name as stated above.
While many of you who are reading this letter have no affiliation with DMR, as taxpayers in this state, you are our partners. This name change is a simple gesture, but a powerful one that demonstrates our respect for people with developmental differences. Please join us as we change the name to show that Massachusetts is a state that does not tolerate offensive or deficit-based labels for people who receive public services.
LAUREL PELTIER
Palmer, Massachusetts
The writer is president, Western Mass. Subcommittee Central/West Regional Citizen Advisory Board, Department of Mental Retardation.
----------
-

-
"Answers on autism"
Updated: 05/23/2008 06:47 AM
By: Ryan Burgess, Capital News 9
HANCOCK, MA. -- "He just became a totally different kid. Communication decreased, {he} screamed, didn't want to go to sleep. When he did sleep, he wanted to be surrounded so he'd sleep on the floor, surrounded by his bed,” said Stacey Ahlman.
She's talking about her 17-year-old autistic son, Taylor. Like many other children across the country, his disorder was misdiagnosed for years.
"I was always just sad. What is it that they're not seeing? What is it that I'm not seeing? Are we doing something wrong? You start to blame yourself sometimes," said Ahlman.
The answer to those questions came when Taylor was finally diagnosed with autism in his teens. Now, other parents like Stacey who have questions about how to better understand and treat the disorder, are learning more at a conference on Autism Spectrum Disorder in Hancock.
"We hope to accomplish a way of honoring children with autism for their own uniqueness and their specialness. And then, also to brainstorm some ways we can make their lives easier, that we can match them on their ground, so we can give them some skills they need to be able to deal with the real world in which they find themselves," said psychologist Helen Bray- Garretson.
More children are diagnosed with autism than cancer, diabetes and AIDS combined. Officials here say that equates to roughly one out of every 150 kids in America.
"Those numbers are recent. About five or ten years ago, those numbers were very different. That might have been one out of 10,000, or maybe then it was one out of 1,000," said Hillcrest Educational Center Learning Director Michelle Morin.
Higher numbers , thanks to increased autism awareness and fewer misdiagnosed disorders, is a concept parents like Stacey Ahlman know all too well.
-
Answers on autism:
Raising a child with autism can pose a number of challenges for the entire family. But as Ryan Burgess tells us, a group of leading autism experts are talking about new ways to support, teach and treat children dealing with the disorder.
-
http://capitalnews9.com/content/headlines/116641/answers-on-autism/Default.aspx
-
----------
-

-
Though Christina DaCruz (right) sought treatment for her alcoholic daughter, Tina Wambolt, Wambolt spent six days at MCI-Framingham before a bed opened at the treatment facility. (Mark Wilson/Globe Staff)
-
"For women addicts, jail can replace treatment: Some sent for care must wait at prison"
The Boston Globe, May 15, 2008
-
This story was written by Globe correspondents Kelsey Abbruzzese, Brittany Peats, and Jordan Zappala.
-
Tina Wambolt knew she needed help battling her alcoholism. What she didn't need were strip searches and a cell in the Framingham women's prison.
Wambolt, 33, of Ashby, fell through a crack in the Massachusetts legal system, into a gap that routinely sends women with serious alcohol or substance abuse problems to the women's state prison when no beds are available in treatment facilities.
"They treat you awful, you feel physically violated, and it's just hell. I shouldn't have had to do that," Wambolt said. "I'm not a criminal."
Wambolt's ordeal last September was triggered by a Massachusetts law known as "Section 35," a civil statute under which a person can be involuntarily committed for up to 30 days if a judge rules that he or she poses a threat to himself, herself, or others.
Men who are civilly committed in Massachusetts are sent to a treatment facility on the grounds of MCI-Bridge water that is large enough to house 250 men, and has not resulted in space issues.
However, a chronic shortage of beds for women in the same circumstances means that some civilly committed women are sent to MCI-Framingham, the state's only women's prison.
During 2007, 14 women, including Wambolt, spent time behind bars during their civil commitments for no reason other than lack of space at a treatment center in New Bedford, the only center in Massachusetts dedicated to Section 35 civil commitments for women. Twenty-seven other civilly committed women were sent to MCI-Framingham last year for refusing treatment or other noncompliant behavior, according to the state Department of Public Health.
During the past five years, according to the state Department of Correction, more than 500 civilly committed women spent a few nights to a few weeks at the prison for reasons ranging from a shortage of treatment beds to behavioral issues. A breakdown was not available to determine how many were sent to the prison solely for lack of space.
Jim Kenney, program director at the New Bedford center, said he works closely with court clinicians, who advise judges on civil commitments, and does what he can through training and working with court officials to keep women from spending time in prison rather than at his facility, a gleaming, recently renovated section of an old mill complex off Interstate 195. Before the New Bedford center opened, women committed under Section 35 were sent to smaller facilities even more pressed for space. He pointed to figures showing that since the 84-bed center's opening in 2006, the number of civilly committed women sent to the prison has fallen sharply. From fiscal year 2006 to 2007, that number dropped by more than two-thirds.
But, as Wambolt's mother, Christina DaCruz, put it, "One is too many."
Watching a child's downfall
DaCruz began the civil commitment process when she went to Wambolt's home after her daughter was arrested for drunken driving. When DaCruz arrived, she said, the house reeked and her daughter had been drinking.
"She looked like someone walking in quicksand," DaCruz said. "This is my baby, my beautiful baby. To have seen her go so far down, I'm like, 'I can't stand this.' "
DaCruz said she had previously persuaded Wambolt to go to a 72-hour hospital detox, but her daughter had started drinking the day she was released. After Wambolt threatened suicide, DaCruz filed a civil commitment petition.
At Wambolt's hearing on Sept. 4 last year, the court clinician who examined her - Wambolt did not recall his name, and civil commitment records are sealed - told DaCruz that her daughter was committable, but would have to stay overnight at MCI-Framingham because there were no beds available in New Bedford.
DaCruz said the clinician told her not to worry, because her daughter would be moved the next day and kept away from the general population of convicts. With those reassurances, DaCruz went ahead with the commitment.
Wambolt recalls little of the hearing. "I remember being in court, but it was kind of a blur," she said. "I was kind of in shock."
Wambolt's husband, Brian, said he called MCI-Framingham every day from Sept. 5, the day after her hearing, until Sept. 8. That day, he said, a prison guard told him that his wife had been moved into the prison's general population.
Diane Wiffin, the state Department of Correction's director of public affairs, wrote in an e-mail that Wambolt was housed and treated in accordance with state law. In the same e-mail, prison Superintendent Lynn Bissonnette wrote that standard practice for women committed under Section 35 is to have them medically detoxed until cleared by a physician. Then they are housed in an area of the prison for women awaiting trial - not among convicted criminals - in a cell alone, or with another woman who has been civilly committed.
That made little difference to Wambolt. "It's like you see on TV. It's prison," she said.
Wambolt is 5 feet, 1 inch tall and weighs 110 pounds, with a pixie haircut and a nose piercing, and her mother and her husband worried for her safety. Wambolt said her cell was next to a woman accused of killing her baby. She added that two other women who were sent to MCI-Framingham for civil commitments spent time in solitary confinement.
"I was threatened to be beaten up," Wambolt recalled. "I was tired and you're stuck there and you swear you just become one of them."
MCI-Framingham's substance abuse program is available only to convicted criminals, so Wambolt and other women waiting to go to treatment centers found themselves in limbo. They received medicine to help them detox, but were ineligible for counseling or other addiction treatments that are available at the New Bedford center. Bissonnette wrote in the e-mail that civilly committed women are ineligible for the prison's treatment program so the prison can "transition them to a community setting as soon as possible."
Five days after the commitment hearing, DaCruz visited her daughter in prison.
"Of course I start crying," DaCruz said. "You have to fill out a paper about why you're there and the guard at the window read the paper and said, 'You know, it happens all the time. People send their family in for committals and they just get lost.' "
Wambolt finally reached the New Bedford treatment center on Sept. 10 - six days after her commitment hearing. DaCruz, who said she believes the transfer happened because of her frantic phone calls, said she was told by an official with the state Department of Public Health, which oversees the New Bedford center, that the center had not been aware of her daughter's existence until the phone calls.
Once she arrived at the New Bedford center, Wambolt said, she saw eight empty beds. Wambolt added that she had to spend more time in intensive detox because of the drugs given to her for medical detox at the prison.
Wambolt is not alone. A woman identified in state Department of Public Health documents as Debra P. entered MCI-Framingham as a civil commitment from the Cambridge District Court on July 18 last year. According to Department of Public Health records, she was sent to prison because there were no open beds in New Bedford. She spent 15 days at MCI-Framingham before being transferred to the center.
Trina P. did not even see the New Bedford facility. When she was committed on Sept. 27 last year, she, too, was sent to MCI-Framingham because of a lack of bed space. Department of Public Health records show she was released from the prison nearly a month later, on Oct. 24, when her commitment expired, having received none of the benefits offered at the New Bedford center.
Legislators hoping to stop civilly committed women from spending time in prison have fought a fruitless battle. Since at least 1989, Massachusetts lawmakers have proposed eliminating MCI-Framingham as a civil commitment option, which would require that women like Wambolt who face no criminal charges are sent to a treatment center. Other bills have sought to extend the time women spend in a treatment center under Section 35. But each year, these bills have failed to win passage and women like Wambolt end up behind bars.
"They haven't committed a crime," said Representative Kay Khan, a Newton Democrat who is the House sponsor of the bill. "Why should they be in a prison?"
Khan, who worked as a clinical psychiatric nurse specialist, said she hopes that the Patrick administration will support the bill and that the departments of Correction and Public Health will provide funding for added beds.
"People need to understand that these people come back out into our community and it really is a public safety issue," she said.
A kinder treatment
Wambolt said she was treated successfully at New Bedford. She said that other than her intensive detox, "It was heaven."
"Nobody strip-searched me, nobody's out there screaming at you, nobody's going to beat you up," she said. "Nobody's mean to you. They really do try to help."
At the center, intensive detox can last from three to seven days. The women sleep in barracks-style rooms with three other patients. There is no furniture except for four bolted-down twin beds. After detox, the women are moved to a Structured Outpatient Addiction Program. For the remainder of the 30-day treatment, they attend seven meetings daily, including lectures on after-care options, Kenney said.
Wambolt added that she is recovering, seeing addiction counselors, and working through an after-care program. Still, her mother bears guilt, and Wambolt bears resentment. As she put it, she was treated like a criminal rather than a woman suffering from a disease.
"I don't even know how the hell we got through that," she said.
-
Kelsey Abbruzzese, Brittany Peats, and Jordan Zappala are graduate journalism students at Boston University. They researched and wrote this story under the supervision of BU professors Dick Lehr and Mitchell Zuckoff, former members of the Globe Spotlight Team.
-
www.boston.com/news/local/articles/2008/05/15/for_women_addicts_jail_can_replace_treatment/
-
------------
The New Hampshire Union Leader, Page B8, “VETERANS”, Edited by Greg Andruskevich, Thursday, May 29, 2008
“House adds Shea-Porter mental health benefit”
Washington—Representatives Carol Shea-Porter, D-N.H., & Patrick Kennedy, D-R.I., successfully added an amendment to the National Defense Authorization Act for Fiscal Year 2009 (H.R. 5658). The amendment will make it easier for service members to get mental health treatment within the military health care system.
“This provision will connect our Reservists with the behavioral health care they need and deserve,” said Shea-Porter, a member of the House Armed Services Military Personnel Subcommittee. “This new pilot program fulfills a promise we have made to service members and their families. I am proud to stand with Representative Kennedy in offering this amendment.” The Kennedy/Shea-Porter amendment requires the Secretary of Defense to create and implement a program to provide a hotline—open 24 hours a day, 7 days a week—to help service members locate behavioral health care providers and schedule appointments within the TRICARE Reserve system.
“We need to be doing everything in our power to make it easier for our troops to get the care they need,” said Kennedy. “Our amendment provides an additional tool that will make it easier to find a mental health professional and schedule that first appointment,” said Kennedy.
A recent study from the Rand Corporation reported that RESERVE MEMBERS OF THE ARMED FORCES ARE AT A HIGHER RISK TO SUFFER FROM DEPRESSION, POST TRAUMATIC STRESS DISORDER, SUBSTANCE ABUSE PROBLEMS, AND OTHER BEHAVIORAL HEALTH ISSUES. The bill passed the House.
The National Defense Authorization Act authorizes funding for the Department of Defense.
Meanwhile Democratic senatorial candidate Jeanne Shaheen stated “I want to congratulate the New Hampshire veterans who have worked so hard on this issue over the past months. Your work in support of this new GI Bill has been influential and I am thrilled to see the bill pass the Senate.
“We should never tell a single veteran that we cannot provide him or her with the resources they need to get a good education. The brave men and women of our armed forces put their lives at risk for each and every one of us in this country and they deserve nothing less than our full admiration, respect and support. In the Senate, I will be a tireless advocate for veterans’ benefits because I believe it is a fundamental American value that we stand up for those who have stood up for us.”
------------
The Boston Globe, Op-Ed, CHRISTOPHER LANE
"Shyness or social anxiety?"
By Christopher Lane, June 11, 2008
THE SOCIETY of Nuclear Medicine has been touting a new study that suggests we're one step closer to solving the riddle of social anxiety disorder. Researchers believe the origins of the disorder are biological.
This sounds like a breakthrough worth celebrating. "Social anxiety disorder affects approximately 15 million American adults," the press release declares, and is "the third most common mental disorder in the United States, after depression and alcohol dependence." But what are its symptoms? A "fear of being evaluated by others, with the expectation that such an assessment will be negative and embarrassing."
At this point, a little voice in my head piped up: "That sounds a tad on the all-inclusive side. Maybe someone has moved the goalposts a bit too far."
Once you start calling fear of criticism a psychiatric disorder, it's easy to ignore the countless social and psychological factors that cause stress and anxiety. Yet the justification for calling the disorder biological turned out to be modest at best. MRI scans of five women and seven men who met the criteria for social anxiety disorder suggested that minor fluctuations of dopamine and serotonin "may play a role in the neurobiology of social anxiety disorder."
That's a bit like saying, "Exercise will increase your heart rate" or "Caffeine is a stimulant." Microscopic fluctuations of dopamine and serotonin impact the brain all the time, helping determine our moods. It's a stretch to predict the health of 15 million Americans from a brief focus on only a dozen of them.
The biggest problem with such claims is that they embrace, rather than narrow, the disorder's amazingly open-ended definition. The Diagnostic and Statistical Manual of Mental Disorders, the world's psychiatric bible, lists as a symptom "fear that the individual may behave in a manner that will be humiliating or embarrassing." If you need a reminder of what such fears are like, think back to the night of your senior prom.
When social anxiety disorder and shyness move so close that it is tough to tell them apart, "meeting the criteria" for the disorder becomes alarmingly easy. That's a key reason the American Psychiatric Association warns practitioners about the risk of misdiagnosis. Shyness is not social anxiety disorder, the latest issue of the Diagnostic and Statistical Manual insists, even after listing symptoms (including public-speaking anxiety) that imply exactly the opposite. Meanwhile, researchers continue to tie the disorder to fear of taking a test, unease about calling someone you don't know, and nervousness about "trying to pick up someone."
These criteria put the risk of misdiagnosis and overmedication distressingly high. The Archives of General Psychiatry reported in 2005, "About half of Americans will meet the criteria" for a Diagnostic and Statistical Manual diagnosis at some point in their lives. True enough, diagnoses of some mental disorders among children have surged by more than 4,000 percent, and nearly a quarter of the US population - 67.5 million - have taken antidepressants.
These figures should cause astonishment across the mental-health professions, as well as an immediate reassessment of the markers used to gauge psychiatric illness. Instead, concern about overdiagnosis has led to defensive posturing, heightened calls for medication, and insistence that experts can pinpoint the line between normal behavior and psychiatric illness. But the authors of "Social Anxiety Disorder: A Guide" state almost casually, "Where shyness ends and social anxiety disorder begins isn't clear. Some social anxiety disorder is expected in everyone." That's exactly the point and precisely the problem.
In preparation for its fifth edition of the Diagnostic and Statistical Manual, due to appear in 2012, the American Psychiatric Association has begun to review its criteria. To restore public and professional confidence in the manual, the organization needs to raise, not lower, its diagnostic thresholds and delete every reference in the manual to mild or routine suffering, so that it's possible once more to distinguish between the chronically ill and the worried well.
Today's turbulent times give us reasons enough to be anxious. The risk of being labeled mentally ill for fearing criticism should not be one of them.
-
Christopher Lane, a professor of English at Northwestern University, is author of "Shyness: How Normal Behavior Became a Sickness."
-
------------
Autism news articles:
www.boston.com/lifestyle/articles/2008/06/07/siblings_of_autistic_children_get_chance_to_express_concerns
&
www.boston.com/bostonglobe/editorial_opinion/letters/articles/2008/06/11/the_conflicts_of_having_an_autistic_sibling/
------------
(A Boston) GLOBE EDITORIAL
"Help for mentally ill children"
June 26, 2008
IN THE universe of worries that parents of mentally ill children face, a needlessly vexing one is the inadequacy and unpredictability of care in hospital emergency rooms. Some children in psychiatric distress get stuck in emergency rooms for days because there are no available beds. Some children are sent home. Some are locked in rooms. And there is no central way - no one phone number or website - for emergency room staff to find beds. Instead, they call around to different psychiatric facilities.
As the Globe's Carey Goldberg reported recently, a dozen children faced such delays in recent weeks. Lisa Lambert, executive director of the nonprofit Parent/Professional Advocacy League, a mental health organization, says she has heard of 30 cases in the last six weeks. No state data are available.
These emergency room traffic jams are part of troubling national trends. Earlier this year, the American College of Emergency Physicians branded "boarding," the warehousing of patients in emergency rooms, as a national problem of overcrowding.
Massachusetts ought to begin tackling this complex problem and take other steps to help families with mentally ill children. In the short term, the state Department of Mental Health could set up a website or a hotline to track psychiatric beds, so that children in distress can be placed rapidly.
And that should be only one modest step in a larger overhaul of the state's public and private mental health resources.
When treatment comes too late
Children who get tardy treatment or none at all end up straining the resources of their families, schools, and communities. In 2001, then-Surgeon General David Satcher issued a report saying that "the burden of suffering experienced by children with mental health needs and their families has created a health crisis. . ."
Satcher called for a community health system - a grand vision of world-class care that would include prevention and early detection of mental illness. Frontline responders such as school teachers, daycare providers, and emergency room workers would be trained to respond to behavioral problems and mental illness. Schools could no longer duck the issue, as parents have sometimes found they do. Wide-ranging research would explore medical, ethical, and logistical issues. There would be better training for mental health professionals and multidisciplinary programs for healthcare professionals that would focus on children's mental health.
Massachusetts is moving in this direction, thanks to the "Rosie D." lawsuit. Filed in 2001, the suit claimed that the state had violated federal law by failing to provide early screening and diagnostic services. Judge Michael A. Ponsor called state efforts "woefully inadequate."
Now the state is implementing a court-approved remediation plan. The first step is under way: Pediatricians are screening Medicaid patients for behavioral and emotional problems. By Nov. 30, the state is supposed to develop a standardized way to assess children with mental health needs. And Nov. 30 is also the deadline for setting up a Web-based system to track care. By June 30, 2009, the state is supposed to have built a network of community service agencies to deliver care to Medicaid-covered children.
A tight deadline
But there are daunting challenges. June 2009 is a tight deadline. And there is a national shortage of children's mental health professionals. To address this, state officials are reaching out to students in clinical programs, encouraging them to become mental health professionals. The state is also developing community college programs to train mental health paraprofessionals. These are sound moves, but they may not be enough to meet the immediate need.
A children's mental health bill on Beacon Hill would pour the foundation for a Satcher-like system for all the state's children. Filed by Representative Ruth Balser, a Newton Democrat, and Senator Steven Tolman, a Brighton Democrat, the bill would promote widespread screening; move "stuck" children out of hospitals and into community programs; and extend insurance to cover "collateral services," such as paying mental health providers to work with doctors and teachers, so that parents don't have to be case managers.
Balser has also filed a mental health parity bill that would help establish better care for children and adults. It is scheduled to be debated in the House today.
A vastly improved mental health system could provide the right care for children at the right time, freeing them and their families to live more productive lives.
------------
"Needless demonizing of mentally ill"
The Berkshire Eagle - Letters
Wednesday, July 09, 2008
I would like to commend Alan Chartock for lending his name, home and considerable clout to the Elizabeth Freeman Center and their upcoming party on July 18. It is indeed a worthy cause, and I hope to attend to add my support to this difficult and untenable situation.
However, I take great exception to Alan characterizing a domestic abuser as an ogre or "a paranoid schizophrenic who would literally kill them." (Eagle, July 5). You do not need to falsely and unjustly drag this much-maligned group of the mentally ill into the gutter to up the emotional ante for the Elizabeth Freeman Center. Doing so simply helps to prolong the myth that people with mental illness are criminally violent, when the truth is that people with mental illness are far more often the victims of crimes then the perpetrators.
The truth, which is even more frightening, is that domestic abusers can be found everywhere, in all social classes, professions and neighborhoods. Yes, some of them may suffer from mental illness, as does about 20 percent of the population. Even so, it is not likely to be from paranoid schizophrenia, a very serious and rare disorder that can cripple its sufferers.
People with mental illness are not ogres. They are people like you and me, people in our families and communities who also deserve our compassion and support. Mr. Chartock, when we have our gala to support families and friends of people with mental illness, I know we can count on your backing. In the meantime, please be careful of what you say. Don't demonize people with mental illness to highlight the needs of abused women. It cheapens their cause and yours.
MOLLY BOXER
Richmond, Massachusetts
The writer is president of the Board of the National Alliance for Mental Illness in Berkshire County.
------------
The Boston Globe, Op-Ed, ROSALYNN CARTER
"A leap in mental care for children"
By Rosalynn Carter, July 10, 2008
IN THE 31 years since I chaired the first presidential commission on mental health, medical science has made significant strides in the diagnosis, prevention, and treatment of mental illnesses. Living in recovery from a mental illness is now not only possible, but expected. Even children and adolescents diagnosed with mental disorders go on to lead healthy, productive lives.
Unfortunately, the nation's social systems for delivering mental healthcare have not kept pace with advances in medical science. There is much more information about how the brain interacts with risk factors for mental illnesses, resulting in effective, evidence-based treatments for depression, ADHD, and even psychosis. But too often these treatments do not reach the people who need them most.
This is especially true for children. National reports estimate that 20 percent of children suffer from mental health problems severe enough to inhibit their ability to learn. However, only one out of five of these children will receive the treatment they need, resulting in more than 50 percent dropping out of school. And suicide remains the third leading cause of death among young people.
Now there is an opportunity to make a dramatic leap forward in expanding access to mental healthcare for all children. At the federal level, Congress is on the cusp of passing landmark parity legislation that would restrict the ability of insurers to discriminate against individuals with mental health and addiction disorders. Although mental illnesses are every bit as real as heart disease or diabetes, insurers have capitalized on the stigma associated with them to limit access to care. The Paul Wellstone Mental Health and Addiction Equity Act would break down the false distinction between mental and physical illnesses and compel insurance companies to treat them equitably.
There are important advances being made at the state level in reforming systems of care. A recent report by Children's Hospital Boston and Massachusetts Society for the Prevention of Cruelty to Children paints a vivid picture of a fractured mental health system that prevents most children, adolescents, and families from getting the care they need.
That report has helped galvanize a large coalition of families, youth, advocates, and providers in support of "An Act Relative to Children's Mental Health" that would create a comprehensive and coordinated system of evidence-based mental health prevention, diagnosis, and treatment that is accessible to all children, adolescents, and families.
The legislation would help ensure the early identification of children with developmental and mental health problems by promoting screening by pediatricians. The earlier that signs of mental illness are identified, the more effective we are in treating the disease, preventing the emergence of more serious conditions, and helping children get back on a path of normal development.
The bill recognizes how vital schools are in reaching children with mental illnesses. By providing mental health consultation services to schools, the bill empowers educators to better understand what may be happening in their students' lives and to identify and respond to early signs of trouble.
It also is important that children are treated in a setting that is appropriate for the level of care they require. Too many children wind up in hospital psychiatric wards because there is no room in residential or community programs or because state agencies cannot agree on who should pay. This bill would facilitate children being moved into more appropriate settings where they could resume attending school and other activities.
There are also thousands of children in the care of state agencies. Currently, several agencies have overlapping responsibility for providing mental health services, which can lead to children receiving multiple and conflicting diagnoses and treatment plans. The Massachusetts bill would designate the Department of Mental Health as the lead agency in designing, delivering, and coordinating services for children.
Just as Massachusetts is the national leader in expanding health insurance coverage to all its citizens, the Massachusetts Legislature can create a model system of children's mental healthcare. This bill points the way toward a system that is comprehensive, collaborative, coordinated, and cost-effective. It would help children experience all the joys of childhood and reach their full potential.
-
Rosalynn Carter, former first lady, is chairwoman of the Mental Health Task Force at The Carter Center in Atlanta.
-
------------
-

-
Senator James Marzilli appeared with his wife Susan at his arraignment in a Lowell court yesterday. Marzilli pleaded not guilty. (BOB WHITTAKER/THE LOWELL SUN VIA ASSOCIATED PRESS)
-
"Marzilli has bipolar disorder, lawyer says: Senator accused in groping case"
By Christopher Baxter, (Boston) Globe Correspondent, July 10, 2008
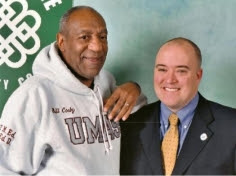
LOWELL - A lawyer for state Senator J. James Marzilli Jr. said yesterday that his client has been diagnosed with bipolar disorder, but he declined to provide any medical specifics.
Speaking after Marzilli's arraignment in Lowell Superior Court, lawyer Terrence W. Kennedy of Everett would not say when Marzilli was diagnosed or discuss how the condition might be related to charges that he groped four women last month in downtown Lowell.
"I've confirmed that he has been diagnosed with a bipolar condition," Kennedy told reporters without elaborating.
Wendy Murphy, a lawyer representing an Arlington woman who told authorities she was groped by Marzilli in a separate case, said any medical condition is no excuse for the alleged criminal actions.
"A lot of people have bipolar disorder, and they don't hurt others," said Murphy. "And they certainly don't assault women in a sexual way, especially in such a prolific sexual way in the course of several years. If he thinks that's somehow justification for his behavior, he's wrong."
At his arraignment, Marzilli stood before Judge Paul A. Chernoff with his hands folded. He pleaded not guilty to charges of annoying and accosting a person of the opposite sex, attempting to commit indecent assault and battery, disorderly conduct, and resisting arrest.
A Middlesex County grand jury indicted Marzilli on the charges July 1.
Kennedy vowed to fight the accusations, questioning their factual and constitutional basis.
He told reporters before the arraignment that he has been told that one of the victims who initially accused the Arlington Democrat of groping her did not support the allegation during grand jury testimony.
He said he expects to file a motion asking the judge to dismiss the most serious charge, indecent assault and battery.
Kennedy said he also expects to challenge the constitutionality of the charges of annoying and accosting people of the opposite sex on the basis that they would not apply to people of the same sex who might engage in the identical offense.
"There will be a number of motions to dismiss that I anticipate will be successful," Kennedy told reporters after the hearing.
The state senator left the courthouse without speaking to reporters.
He walked hand in hand with his wife, Susan Shaer, who is executive director of Women's Action for New Directions, an antiwar group.
They got into a white Toyota Prius and drove away.
Marzilli is scheduled to return to court July 28.
The veteran lawmaker is accused of attacks occurring over four hours on the afternoon of June 3.
Marzilli was detained that day after leading police on a foot chase. Days later, he checked into McLean Hospital.
Marzilli has been free on $1,500 cash bail since pleading not guilty at an arraignment in Lowell District Court on June 4.
Chernoff agreed yesterday to transfer the bail to superior court under the condition that Marzilli stay out of Lowell and have no contact with the four alleged victims.
Marzilli, who served for 17 years in the House before being elected to the Senate in a special election last year, has said he will not run for reelection this fall.
He was facing two Democratic opponents and had been considered certain to win the seat.
-
Christopher Baxter can be reached at cbaxter@globe.com.
-
------------
"State bond will allow for more renovations"
By Jack Dew, Berkshire Eagle Staff
Monday, July 14, 2008
STOCKBRIDGE — As it pushes toward the completion of a major upgrade to its Main Street campus, Austen Riggs has secured a $4 million bond from the state that will carry low interest and no taxes for the psychiatric hospital.
The bond will finance the ongoing renovation of the 89-year-old institution that offers patients residential and outpatient treatment. It is the second $4 million bond that Austen Riggs has received from the Massachusetts Health and Educational Facilities Authority, or HEFA, a quasi-public agency that provides low-cost funds to nonprofit organizations throughout the state.
Chauncey Collins, director of operations and finance at Austen Riggs, said the money will help connect the residential housing facility to the newly built community center, which includes a communal kitchen, lounge area and fitness center, allowing inpatients to mingle with those who have stepped down their treatment and are living off campus. The two buildings will be joined by a 1,000-square-foot porch and lobby.
"It's very significant," Collins said of the $4 million bond. "These are big numbers. Our annual budget is about $16 million, so it is a significant part of our longer range planning."
The money will also be used to upgrade the Inn, where many of the 75 inpatients live. The hospital plans to improve the electrical system, add air conditioning, and install an elevator in the historic building, which was built in the 1890s and remains a handsome landmark along Stockbridge's iconic Main Street.
The earlier bond, issued in 2004, was used to renovate Lavan Hall and to acquire and renovate a residential program in Lenox. Austen Riggs will pay 5.09 percent interest on the new bond — which will be placed with Lee Bank — over 20 years.
These bonds "are a very efficient way for smaller nonprofits to access the tax-exempt market," said Benson T. Caswell, HEFA's executive director. "This financing will allow Austen Riggs to meet its own improvement goals, while avoiding the extra costs associated with commercial or taxable debt."
State Rep. William "Smitty" Pignatelli, D-Lenox, said Austen Riggs "is a real asset to the whole area, and they've been a good neighbor. This financing further solidifies their presence here in the Berkshires and allows them to continue doing the great work that they do."
State Sen. Benjamin B. Downing agreed, saying its "world-class psychiatric care" has enriched "the lives of so many."
"This much-needed funding will allow Austen Riggs to improve their infrastructure while continuing their tradition of exceptional therapeutic treatment," he added.
-
To reach Jack Dew: jdew@berkshireeagle.com (413) 496-6241
-
------------
"Mental health bill costs to be minimal, study says"
By Neil Munshi, (Boston) Globe Correspondent, July 4, 2008
Mental health advocates are praising a state report as validation that a bill expanding mental health care and substance abuse treatment will not be too costly, a chief concern of business and insurance groups.
The Department of Public Health evaluation - based on a review of past studies, an actuarial analysis, and interviews with Massachusetts insurers and providers - projected that the mental health parity legislation, which overwhelmingly passed the House Monday, would add between 0.1 percent and 0.3 percent to the cost of insurance. That works out to between 46 cents and $1.39 per member per month.
"I hope this report finally puts to rest health plan and business concerns that this makes health insurance unaffordable for people," said Marylou Sudders, president and chief executive of the Massachusetts Society for the Prevention of Cruelty to Children and a former state mental health commissioner.
But Dr. Marylou Buyse, president of the Massachusetts Association of Health Plans, said her organization is concerned about adding new benefits amid a slowing economy.
"Percentages are very deceptive," she said, noting that the figures in the report translate into a statewide annual increase of $12.9 million to $38.8 million. "Adding new mandates will increase costs for employers, particularly small businesses, which are the backbone of the Massachusetts economy."
Buyse added that the Commonwealth already has generous mental health benefits, based on a 2000 law that requires insurers to treat certain psychiatric illnesses, including bipolar disorder and schizophrenia, as they do physical ailments, placing no annual or lifetime limits on benefits.
That law, however, still allows limits on hospitalizations and outpatient treatment for dozens of maladies, such as eating disorders, post-traumatic stress, and drug addictions. The new bill, which is awaiting Senate action, seeks to eliminate those limits.
Matthew McKenna - chief of staff for Senator Steven A. Tolman, a Boston Democrat who cosponsored the original bill - said Massachusetts is at the forefront of expanding healthcare coverage and the legislation is a key step in that direction. In light of the DPH report, McKenna said, "the senator is very optimistic that this bill is going to pass."
Correction: Because of an editing error, a story Friday in the City & Region section listed the wrong state agency as the author of a report on the cost of proposed mental health parity legislation. The analysis was prepared by the Division of Health Care Finance and Policy.
-----
"Don't scapegoat mental health"
The Boston Globe, Letters, July 16, 2008
ON JUNE 23 the Massachusetts House of Representatives enacted comprehensive mental health parity in health insurance coverage over the objections of health insurers and others who warned of high costs. An actuarial analysis released shortly after the vote concluded what many had predicted: The projected increase in cost is minimal - somewhere between 0.1 percent and 0.3 percent. ("Mental health bill costs to be minimal, study says," July 4, Page B6).
Almost all agree that mental health and substance abuse treatments have little, if anything, to do with the rising costs of healthcare and healthcare insurance. Others point to trial lawyers and defensive medical practices adopted to minimize the risk of excessive malpractice awards as major culprits. But while no one claims treatment for mental illnesses or substance abuse disorders are the cause, guess who some are asking to be thrown under the bus?
The Senate should follow the House's lead and enact mental health parity, and the House should follow the Senate's lead and enact legislation addressing healthcare cost containment.
Continuing to allow insurers to treat healthcare coverage for mental illnesses and substance abuse disorders differently than all other illnesses will not address the real issues, and it will continue to discriminate against citizens of the Commonwealth with real, treatable illnesses.
BERNARD J. CAREY JR.
TIMOTHY O'LEARY
The writers are executive director, and deputy director for policy and research, respectively, at the Massachusetts Association for Mental Health.
------------
"Mental illness doesn't discriminate" - The North Adams Transcript - Letters, Thursday, September 18, 2008
To the Editor:
Mental Illness Awareness Week is Oct. 5 to 11. That same week, our presidential candidates will hold a "town hall" debate -- in which up to a quarter of the audience are likely to have experienced a mental illness.
That's because one in four adults lives with depression, bipolar disorder, schizophrenia, post-traumatic stress disorder (PTSD) and other mental illnesses every year. That's almost 60 million Americans.
Mental illness does not discriminate between Republicans and Democrats. It can strike anyone at any time.
Mental health is part of health care and it is essential that it be included in the nation's health care reform debate.
Mental illness affects children. It affects people of color. Two million Americans live with schizophrenia--twice the number of those with HIV/AIDS. One in five veterans of Iraq and Afghanistan--almost 300,000 troops--will experience major depression or PTSD upon returning home. Unfortunately, two-thirds of people who live with mental illnesses do not receive treatment.
But treatment works. Recovery is possible. Between now and Election Day, every candidate needs to talk about these facts.
For more information, contact the National Alliance on Mental Illness of Berkshire County at 413-443-1666 and e-mail: namibc @namibc.org or visit www.nami.org.
Mary Rowland
North County coordinator, child/adolescent specialist
National Alliance on Mental Illness of Berkshire County
333 East St.
Pittsfield, Massachusetts
------------
"Mental illness must be election issue"
The Berkshire Eagle - Letters
Monday, September 29, 2008
Mental Illness Awareness Week is October 5-11. That same week, our presidential candidates will hold a "town hall" debate in which up to a quarter of the audience are likely to have experienced a mental illness. That's because one in four adults lives with depression, bipolar disorder, schizophrenia, post-traumatic stress disorder (PTSD) and other mental illnesses every year. That's almost 60 million Americans.
Mental illness does not discriminate between Republicans and Democrats. It can strike anyone at any time. Mental health is part of health care and it is essential that it be included in the nation's health care reform debate.
Mental illness affects children. It affects people of color. Two million Americans live with schizophrenia, twice the number of those with HIV/AIDS. One in five veterans of Iraq and Afghanistan — almost 300,000 troops — will experience major depression or PTSD upon returning home.
Unfortunately, two-thirds of people who live with mental illnesses do not receive treatment. But treatment works. Recovery is possible. Between now and Election Day, every candidate needs to talk about these facts.
For more information, contact the National Alliance on Mental Illness of Berkshire County at (413) 443-1666 and e-mail: namibc @namibc.org or visit HYPERLINK "www.nami.org."
MOLLY BOXER
The writer is president of the Board of Directors, National Alliance on Mental Illness of Berkshire County.
Pittsfield, Massachusetts
------------
-

-
Pittsfield Mayor James M. Ruberto, right, speaks during the candlelight vigil at Berkshire Medical Center in recognition of Mental Health Awareness Week. (Caroline Bonnivier / Berkshire Eagle Staff)
-
"Mental Health Awareness Week: Fight is on to remove a stigma"
By Jack Dew, Berkshire Eagle Staff, Wednesday, October 08, 2008
PITTSFIELD — No one, Dr. Kenneth Duckworth said, gets flowers and casseroles when they come home from a psychiatric hospitalization.
Discussing the disparity between mental health care and general medicine in the country, Duckworth said the bias against mental illness goes beyond the institutions — hospitals, insurance companies, states — and encompasses society.
Speaking at Berkshire Medical Center last night, Duckworth — the medical director of the National Alliance on Mental Illness and an assistant professor at Harvard University Medical School — said the nation is working with a "very broken and underfunded system," where the seriously ill, suffering from schizophrenia, depression, bipolar disorder and other conditions, face barrier after barrier as they and their families seek treatment.
"People don't get tuna casserole after a psychiatric hospitalization. They just don't," Duckworth said. That is indicative of an "absence of social lubrication. Nobody knows how to take this on, so they just ignore it."
That same ignorance is found in the medical field, he said. When patients taking psychiatric medication gained weight, doctors turned a blind eye. That in turn led to higher cholesterol and increased risk of diabetes among the mentally ill, who often smoke as a means of coping and who often live under high stress. The result: a substantially increased risk of heart disease, costing an average of 16 to 18 years off a patient's life.
"Most of these risks are conditions we can treat, but there has to be a system to treat them, and for that, we have to have advocacy," he said.
A report by the National Alliance on Mental Illness — or NAMI — that graded all 50 states found these systems critically lacking; Massachusetts fared better than many, but still received a "D."
Duckworth's talk was sponsored by NAMI of Berkshire County, which is dedicated to increasing awareness about mental illness and advocating for reform, and came during Mental Illness Awareness Week.
After his address, the Berkshire chapter held a candlelight vigil in the hospital courtyard. As three dozen people stood in a circle, Mayor James M. Ruberto read a proclamation urging greater awareness and understanding of mental illness.
Molly Boxer, president of the Berkshire County chapter, said there has been progress: In Massachusetts, new legislation may boost children's mental health, and the just-passed federal bailout was attached to a bill that will require insurance providers to cover mental health as they do other health problems. But there is still a long way to go.
Her nephew suffered a head injury in an accident, she said. He got family support, community support and insurance support. "My son, who has a mental illness, got none of that. The difference was so stark."
Amy Alexander said she was diagnosed with a mental illness in 1986. Now she participates in the "In Our Own Voice" program, traveling the county to address groups and discuss her experience.
While she said the treatment in the Berkshires has been strong, with Berkshire Medical Center and its Jones unit as a pillar, "we still have a long way to go. We have a long way for the stigma to disappear."
-
To reach Jack Dew: jdew@berkshireeagle.com 413) 496-6241
-
------------
"Reference to autism puzzling, disturbing"
The Boston Globe Online - Letters, October 17, 2008
AS A former teacher of children with moderate learning disabilities, and a former special education administrator, I winced during the debate Wednesday between Senators Barack Obama and John McCain when the latter, emphasizing his empathy for such children, commented that he'd increase funding for autism research. I wondered: Is he obliquely referring to Governor Sarah Palin's youngest child, who has Down syndrome and who likely will need extra support in his schooling? Or is he conveniently choosing to emphasize a condition that he is more aware of as it has gained much press based on the rapid rise in diagnosis in the last decade? Surely, McCain could not confuse autism with Down syndrome. Yet sadly, that is what he appeared to do, as later in the debate, he cited Palin as one who could relate "better than most" to parents of autistic children and their educational funding needs.
I gave McCain a pass on the first comment, but must now ask: How well can he know Palin and her family to not know that there are major differences between autism and Down syndrome?
I don't expect McCain to know genetics or neurology, but perhaps he should understand more of the complexities of educating all children before he lectures on the benefits of education reform and the subsequent changes in funding, and restructuring at the local level, that he proposes.
ANNE MARIE FLYNN
Hopkinton, Massachusetts
------------
"Words working backwards: A psychologist explains learning disorders from his own experience."
By Jenn Smith, Berkshire Eagle Staff, Wednesday, December 03, 2008
PITTSFIELD — Learning disorders can be complex in origin and definition. But at Tuesday's Hillcrest Educational Centers conference on the topic, they were summed up on the side of a candy bar.
Each of the 135 participants yesterday were given a familiar-looking chocolate bar in dark mocha-colored wrapper. But instead of the bold-faced silver lettering reading "Hershey's," for example, the bar was labeled "Dyslexia."
Printed beneath it were the "ingredients": Neurological in origin, difficulties with accurate and/or fluent word recognition, poor spelling and decoding abilities, problems in reading comprehension, reduced reading experience, etc.
"The important thing for society to remember is that these are invisible disabilities. People don't choose to have these disorders. A child doesn't want to be dyslexic. There is a neurobiological reason for it," said Dr. Kevin Blake.
Blake was the key speaker at the conference giving a presentation titled "I Pulled an All-Nighter for My High School Graduation and Other Adventures of a Hearing-Impaired, Dyslexic Psychologist."
Indeed, Blake was inspired to pursue a career as an authority on learning disorders by his own learning disabilities. It was because of lack of understanding and field research that Blake wasn't diagnosed until age 26.
The participants in Tuesday's conference largely included Hillcrest employees, as well as representatives from local private and public schools and parents.
Several people commented on how helpful it was to hear Blake's first-hand experience with learning disorders.
"It helps to see someone who has gone through this in their life. It's a reminder of what we as teachers need to do for our students," said Nicola McMahon, who teaches at Hillcrest's day school program at Housatonic Academy.
According to clinician Thomas Lusignan, clinicians and teachers often work together as a team to tailor interventions for students.
In addition to reading disorders and dyslexia, Blake also spoke about attention-deficit/hyperactivity disorder (AD/HD), the neurobiology of the disorders and both alternative and integrated medical treatments for them.
According to the National Institute of Mental Health, nearly 4 million school-age children have learning disabilities. Of these, at least 20 percent have a type of disorder that leaves them unable to focus their attention.
Blake and conference participants noted how learning disorders can cause a person to be labeled as "lazy" or a "late-bloomer" or worse yet, "an idiot."
"Kids are still absolutely stigmatized. They're seen as trouble, especially if they end up removed from school and coming to us," said Metta Burpee, director of clinical services at Hillcrest.
In some cases, the solution can be teaching a person an alternative way of looking at a math problem or checking to see whether one needs glasses or a hearing aid.
Michele Morin, Hillcrest's director of workforce development, who helped organize the conference, noted that schools are more than ever equipped with knowledge and support and research of learning disorders, but that society at-large is not as informed.
"I've been in classrooms where kids know what other kids have and will work around that," she said. "The real challenge is finding continuing support for adults. We can all do a better job with that."
------------
-

-
Ken and Danielle Lambert of Brentwood, N.H., grieve for their children. (Erik Jacobs for the Boston Globe)
-
"Finding words at last for an unspeakable loss: Parents of two dead children seek to prevent repeat of tragedy"
By Jonathan Saltzman, Boston Globe Staff, December 7, 2008
BRENTWOOD, N.H. - The refrigerator is still covered with red, yellow, and blue magnetic letters and numbers. A Play-Doh set rests atop a wooden kitchen cabinet, as if tiny fingers will play with it soon. Living room shelves are stacked neatly with Candyland, Chutes and Ladders, Barbie dolls, and toy cars.
Eleven months have passed since Danielle and Ken Lambert's 5-year-old daughter and 4-year-old son were carried to their deaths into oncoming traffic on Interstate 495 in Lowell by Danielle's identical twin in a nearly unfathomable tragedy. Yet their belongings still fill their house in this rural town in southeastern New Hampshire.
"I just don't feel like I want to move it," said Danielle Lambert, in a recent interview. "I kind of like keeping things as they were. It sort of gives us a feeling of their presence." Lambert lost not only her only children, but her sister, Marcelle Thibault, on Jan. 11.
The Lamberts's anguish remains raw from that chilly Friday night when Thibault picked up their children to drive to a sleepover with cousins at her house in Bellingham. Along the way, Thibault crossed the median of I-495, stopped her car in the wrong direction, undressed herself and the two children, and then ran them to their deaths. According to one eyewitness, she was screaming about religion before she was hit.
But in the Lamberts's grief, they are searching for whatever clarity they can find and trying to use the information they have begun gathering to prevent the unthinkable from happening to someone else.
The State Police, the Lamberts have discovered, came heartbreakingly close to detaining Thibault for a psychiatric evaluation when they found her behaving erratically hours earlier that night on the median strip of the very same highway. But the three troopers decided against it, and Thibault continued on her way to New Hampshire to pick up her niece and nephew.
The Lamberts said they had no reason to worry when Thibault arrived to pick up Kaleigh and Shane for the sleepover. Thibault, who was 39, had been treated at McLean Hospital four months earlier and diagnosed with bipolar disorder, the couple said. But she seemed nearly fully recovered and was behaving normally when she collected the pajama-clad children, along with their favorite pillows and sleeping bags.
"She was acting like the normal Marci I knew all my life," Danielle Lambert, a 40-year-old pediatric nurse practitioner, said.
Now, the State Police are one of two entities that the Lamberts said share blame for their children's deaths, the other being the renowned McLean Hospital, a Harvard-affiliated psychiatric facility in Belmont. The family believes that the hospital released Thibault far too early, and without any warnings about the risk she might pose to herself or others.
State Police said they acted appropriately in the case, and McLean officials, citing privacy concerns, declined to address the particulars of Thibault's treatment.
"If she got the help she needed, this wouldn't have happened," Danielle Lambert said. "My sister was a good person. She was my best friend. I know she wouldn't have done that intentionally."
Lambert, though, might have barely recognized the woman who police came across on the median strip of I-495 in Andover when Thibault was en route to New Hampshire to pick up the children.
Thibault was punching another motorist - a good Samaritan who stopped to assist her - when State Police arrived around 7 p.m. After that, as troopers questioned Thibault, she splashed her feet in the swampy grass and told a trooper she was having a "debate between good and evil," according to State Police documents that were obtained by the Lambert family and shared with the Globe.
One trooper, according to the records, suggested to his colleagues that she be "pink slipped," or taken for a psychiatric evaluation, according to the reports. Thibault told the officers she was driving to her sister's house and had dozed off. The troopers decided they lacked enough evidence to detain her and issued a ticket for failing to stay in marked lanes.
Two hours later, Thibault carried her niece and nephew into traffic, and those same three troopers raced to the scene. They quickly realized she was the woman they had questioned, according to the reports. Her traffic ticket was still in her car, and the radio was blaring at top volume.
Sitting at her dining room table, her husband holding her hand, a tearful Danielle Lambert said the couple would never have let their children go with Thibault if they had known about her actions earlier in the night.
David Procopio, a State Police spokesman, said recruits undergo training at the police academy for dealing with mentally ill people and continue online training after being sworn in.
The troopers who responded earlier on I-495 behaved properly, Procopio said. They decided not to take Thibault in for an evaluation because she had calmed down after flailing at the motorist who had stopped his car after seeing her drive onto the median at highway speed. (The unidentified motorist called Thibault "crazy," according to police reports, but did not want to press charges). Procopio said Thibault was unimpaired by alcohol or drugs, and that the troopers did not have enough evidence to seek a psychiatric evaluation.
"Like so many parts of a police officer's job, the decision to commit a person who is potentially emotionally disturbed is a judgment call that has to be made after a relatively brief observation period," Procopio said. "They did everything correctly in terms of questioning her and doing their best to obtain information from her."
The Lamberts have hired noted Boston lawyer Andrew C. Meyer Jr., but have not filed a lawsuit. If they do, the likely target won't be the State Police, but McLean Hospital, Meyer said. Massachusetts law makes it extraordinarily hard for plaintiffs to prove liability against police officers in wrongful death claims.
The Lamberts, in the interview, said McLean doctors should not have discharged Thibault after six days; Thibault, they said, was still delusional and believed God had sent her to the hospital to help other patients. Danielle Lambert and another sister, Stacey Coady, also said McLean staff never told the family at a meeting before Thibault's discharge that she was at risk to kill herself or someone else.
The Lamberts have started a nonprofit group, Keep Sound Minds - www.keepsoundminds.org - and want to change how police officers respond to individuals exhibiting serious mental illness. The organization, which is holding a fund-raiser March 28 at the Sheraton Boston Hotel, also wants to change how psychiatric hospitals discharge patients, including requirements to discuss risks of suicide and homicide with family members and to make sure patients get outpatient treatment.
McLean issued a statement that did not address Thibault directly, but said that its clinicians work with patients and their families to educate them about mental illness and devise a treatment plan "to which the patient agrees to adhere as they prepare to return home." The statement said the hospital welcomes suggestions for possible improvements in its procedures.
Dr. Alberto M. Goldwaser, a forensic psychiatrist who teaches at New York University's medical school, said it is understandable that the Lamberts are second-guessing the State Police and McLean. But he said the couple's criticisms are probably unrealistic.
"Right now, we know the police should have taken her to a hospital, and then this tragic event wouldn't have happened. But that's in hindsight," said Goldwaser, who is not involved in the case. "So, yeah, [Thibault] was peculiar. We're talking about taking her liberties, taking her freedom."
If anyone was in a position to gauge whether Thibault appeared to be a danger, he added, it was Danielle and Ken Lambert, and they detected nothing amiss when Thibault arrived. "She shouldn't blame anybody, not even herself," he said of Danielle Lambert. "This kind of horrible event doesn't happen very often."
Thibault's husband, Michael, an EMC Corp. employee who met his wife at Bellingham High School, said it might be a good idea for police to have access to a database of individuals who had been committed to psychiatric hospitals, despite the inherent privacy concerns. He said the State Police "had Marci in their hands on the way up" to New Hampshire.
But Dr. Mark Goldblatt, a Cambridge psychiatrist and president of the New England chapter of the American Foundation for Suicide Prevention, said Americans are ambivalent about how to respond to people with mental illness.
"Society wants it both ways," he said. "We want to have complete freedom and liberty and not be restrained by government, not have people's names in databases. And at the same time, we want to control people who live a certain way with mental illness. It's hard to have both."
Marcelle Thibault and Danielle Lambert were two of eight children, all girls, who grew up in Bellingham. Marcelle graduated from Johnson & Wales University in Providence. She and Danielle were the maids of honor in each other's weddings. In recent years, Thibault worked part-time jobs while raising her two children with her husband.
Since the tragedy, Danielle Lambert and Stacey Coady have learned about a history of mental illness spanning several generations in their family. Although Thibault was sometimes anxious, her twin said, she never displayed any serious mental disorder until September 2007, when she was fired from a custodial job she had held for a few weeks at Bryant College in Smithfield, R.I. "That's what triggered everything," Lambert said. "She was embarrassed, demoralized, and it consumed her."
Thibault would talk to her sister on the phone and rant that she was "good, righteous, and kind" and her former employer was "evil and cold." In one call, she yelled so loudly and rapidly that an alarmed Lambert pulled the phone from her ear, and her co-workers overheard it.
Thibault also began telling people that she had received angel's wings and had been anointed by God to make the world better, Lambert said.
In response to such behavior, Coady and Thibault's husband Michael took her to Massachusetts General Hospital in September 2007 and, from there, she was admitted to McLean. Doctors diagnosed her with bipolar disorder and discharged her six days later after prescribing psychotropic drugs and recommending outpatient therapy, Danielle Lambert said.
Danielle Lambert told doctors before the discharge that she was concerned Marcelle Thibault still seemed to have delusions. But the physicians told her the thoughts were not dangerous and that Thibault could resume her activities, Lambert said.
She did for several months, Danielle Lambert said. She volunteered at a church and behind the concession stand at Bellingham High School football games. She hosted her annual Christmas party. By late last year, Lambert said, Thibault was "95 percent back to her old self." Nonetheless, Thibault's sisters were worried that she had stopped taking medication, declined to go to therapy, and seemed to embrace religion with an unfamiliar fervor.
On Jan. 11, Thibault showed up at the Lamberts's house at 8 p.m., about 90 minutes later than scheduled, to pick up Kaleigh and Shane. Danielle Lambert said she would have driven her children to Bellingham, but was participating the next day in a bone marrow donor drive for a New Hampshire girl with leukemia.
Thibault never mentioned her run-in with the troopers and seemed normal, the Lamberts said. She sipped a cup of tea and watched the end of "Hannah Montana" with the children before loading them into the car and heading to Bellingham, Lambert said.
"Be good for Auntie Marci and Uncle Mike," Ken Lambert recalled telling his children.
Around 10:30 p.m., the phone rang at the Lamberts's house. Danielle Lambert said she had a feeling it was bad news even before a 16-year-old niece told them about the accident.
Since the tragedy, the Lamberts have undergone therapy and met repeatedly with a priest who has comforted them. They discussed the deaths in Washington with congressman Patrick Kennedy of Rhode Island, an advocate for improved mental health care who has bipolar disorder and a history of substance abuse. They said they want to educate people about how deadly untreated mental illness can be.
"I have a lot of questions, of course," Danielle Lambert said, with a catch in her voice, as she showed a visitor Kaleigh and Shane's toys and books. "Why did God let this happen?"
She paused. "I just hope that we will see them again in heaven."
-
Jonathan Saltzman can be reached at jsaltzman@globe.com.
-
------------
JOAN VENNOCHI
"Equality for all"
By Joan Vennochi, Boston Globe Columnist, December 31, 2008
As part of the state budget passed last summer and signed by Governor Deval Patrick, the Department of Mental Retardation was quietly renamed. As of July 1, 2009, it will be called the Department of Developmental Services.
You can call the agency's new moniker a euphemism, and another tedious sign of political correctness.
Or you can call it what its advocates do: a long overdue decision that forces Massachusetts into the 21st century by updating the state's bureaucratic lingo and treating all Bay State citizens with dignity.
"It's about respect," said Ed Bielecki, state coordinator for Massachusetts Advocates Standing Strong, the group that has been working for years to change the name.
"Mental retardation" is currently used as a stand-alone term in the agency titles of only seven states (Alabama, Kentucky, Massachusetts, Mississippi, Pennsylvania, Tennessee, and Virginia).
Twenty-three states use the term "developmental disabilities" as a stand-alone term in their agency titles.
Now, Massachusetts is taking a step beyond that, as it joins with Connecticut and California to take "retardation" and "disabilities" completely out of the agency title.
Advocates have been lobbying state legislators and bureaucrats for about a dozen years, Bielecki said. Two years ago, state Representative Michael A. Costello of Newburyport filed legislation supporting the effort. The Patrick administration got behind it and what had been an uphill battle gained political momentum.
"The philosophy and direction from the top is wonderful and enlightening," said Bielecki.
Commissioner Elin Howe, who heads the newly baptized Department of Developmental Services, said it may be difficult for some to understand the importance, "but it is really significant to individuals who have so long fought for self-respect."
The "Department of Mental Retardation" emphasizes the negative. The "Department of Developmental Services" embraces the possible. If the positive name change is supported by an equally positive agency agenda, it is an important step for Massachusetts.
-
Joan Vennochi can be reached at vennochi@globe.com.
-
------------
"The Mystery of Borderline Personality Disorder"
By John Cloud/Seattle, Thursday, Jan. 08, 2009
Doctors used to have poetic names for diseases. A physician would speak of consumption because the illness seemed to eat you from within. Now we just use the name of the bacterium that causes the illness: tuberculosis. Psychology, though, remains a profession practiced partly as science and partly as linguistic art.
Because our knowledge of the mind's afflictions remains so limited, psychologists — even when writing in academic publications — still deploy metaphors to understand difficult disorders. And possibly the most difficult of all to fathom — and thus one of the most creatively named — is the mysterious-sounding borderline personality disorder (BPD). University of Washington psychologist Marsha Linehan, one of the world's leading experts on BPD, describes it this way: "Borderline individuals are the psychological equivalent of third-degree-burn patients. They simply have, so to speak, no emotional skin. Even the slightest touch or movement can create immense suffering."
Borderlines are the patients psychologists fear most. As many as 75% hurt themselves, and approximately 10% commit suicide — an extraordinarily high suicide rate (by comparison, the suicide rate for mood disorders is about 6%). Borderline patients seem to have no internal governor; they are capable of deep love and profound rage almost simultaneously. They are powerfully connected to the people close to them and terrified by the possibility of losing them — yet attack those people so unexpectedly that they often ensure the very abandonment they fear. When they want to hold, they claw instead. Many therapists have no clue how to treat borderlines. And yet diagnosis of the condition appears to be on the rise.
A 2008 study of nearly 35,000 adults in the Journal of Clinical Psychiatry found that 5.9% — which would translate into 18 million Americans — had been given a BPD diagnosis. As recently as 2000, the American Psychiatric Association believed that only 2% had BPD. (In contrast, clinicians diagnose bipolar disorder and schizophrenia in about 1% of the population.) BPD has long been regarded as an illness disproportionately affecting women, but the latest research shows no difference in prevalence rates for men and women. Regardless of gender, people in their 20s are at higher risk for BPD than those older or younger.
What defines borderline personality disorder — and makes it so explosive — is the sufferers' inability to calibrate their feelings and behavior. When faced with an event that makes them depressed or angry, they often become inconsolable or enraged. Such problems may be exacerbated by impulsive behaviors: overeating or substance abuse; suicide attempts; intentional self-injury. (The methods of self-harm that borderlines choose can be gruesomely creative. One psychologist told me of a woman who used fingernail clippers to pull off slivers of her skin."
No one knows exactly what causes BPD, but the familiar nature-nurture combination of genetic and environmental misfortune is the likely culprit. Linehan has found that some borderline individuals come from homes where they were abused, some from stifling families in which children were told to go to their room if they had to cry, and some from normal families that buckled under the stress of an economic or health-care crisis and failed to provide kids with adequate validation and emotional coaching. "The child does not learn how to understand, label, regulate or tolerate emotional responses, and instead learns to oscillate between emotional inhibition and extreme emotional lability," Linehan and her colleagues write in a paper to be published in a leading journal, Psychological Bulletin.
Those with borderline disorder usually appear as criminals in the media. In the past decade, hundreds of stories in major newspapers have recounted violent crimes committed by those said to have the disorder. A typical example from last year was the lurid tale of an Ontario man labeled borderline who used a screwdriver to gouge out his wife's right eye. (She lived; he got 14 years."
There are several theories about why the number of borderline diagnoses may be rising. A parsimonious explanation is that because of advances in treating common mood problems like short-term depression, more health-care resources are available to identify difficult disorders like BPD. Another explanation is hopeful: BPD treatment has improved dramatically in the past few years. Until recently, a diagnosis of borderline personality disorder was seen as a "death sentence," as Dr. Kenneth Silk of the University of Michigan wrote in the April 2008 issue of the American Journal of Psychiatry. Clinicians often avoided naming the illness and instead told patients they had a less stigmatizing disorder.
Therapeutic advances have changed the landscape. Since 1991, as Dr. Joel Paris points out in his 2008 book, Treatment of Borderline Personality Disorder, researchers have conducted at least 17 randomized trials of various psychotherapies for borderline illness, and most have shown encouraging results. According to a big Harvard project called the McLean Study of Adult Development, 88% of those who received a diagnosis of BPD no longer meet the criteria for the disorder a decade after starting treatment. Most show some improvement within a year.
Still, the rise in borderline diagnoses may illustrate something about our particular historical moment. Culturally speaking, every age has its signature crack-up illness. In the 1950s, an era of postwar trauma, nuclear fear and the self-medicating three-martini lunch, it was anxiety. (In 1956, 1 in 50 Americans was regularly taking mood-numbing tranquilizers like Miltown — a chemical blunderbuss compared with today's sleep aids and antianxiety meds.) During the '60s and '70s, an age of suspicion and Watergate, schizophrenics of the One Flew Over the Cuckoo's Nest sort captured the imagination — mental patients as paranoid heroes. Many mental institutions were emptied at the end of this period. In the '90s, after serotonin-manipulating drugs were released and so many patients were listening to Prozac, thousands of news stories suggested, incorrectly, that the problem of chronic depression had been finally solved. Whether driven by scary headlines, popular movies or just pharmacological faddishness, the decade and the disorder do tend to find each other.
So, is borderline the illness of our age? When so many of us are clawing to keep homes and paychecks, might we have become more sensitized to other kinds of desperation? In a world so uncertain, maybe it's natural to lose one's emotional skin. It's too soon to tell if that's the case, but BPD does have at least one thing in common with the recession. As Dr. Allen Frances, a former chair of the Duke psychiatry department, has written, "Everyone talks about [BPD], but it usually seems that no one knows quite what to do about it."
Inside the Mind
To have coffee with Lily (a pseudonym), you wouldn't get much sense of how she has suffered. She is 40 but could pass for 30. She has blue eyes and long blond hair that falls across her shoulders in slightly curly tendrils. On the December day we met at a diner outside Seattle, she wore a pink wool cap pulled down tight and an Adidas jumper zipped all the way. She was friendly but not terribly expressive, and she carried an aura of self-protection.
At one point in the late '90s, Lily was taking five drugs that doctors had prescribed: three antidepressants, an antianxiety medication and a sleeping pill. Borderline patients are often overmedicated — partly because therapists see them as difficult — but for Lily, as for most borderlines, the meds did little. "Drug treatment for BPD is much less impressive than most people think," Paris writes in Treatment of Borderline Personality Disorder.
As a teenager, Lily felt little self-confidence. "Junior high and high school just sucks, right?" she said, laughing. "But I had a propensity to take it a little more seriously." With the help of therapy, she made it through high school and college, but in her late 20s, she became dissatisfied with her job selling specialty equipment. One October day, as she headed out for a mountain-biking trip, she looked at the dun sky and had the feeling that something was wrong. Bleakness massed around her quickly, much faster than it had when she was younger. Soon, nothing gave Lily much joy.
She recalled a talk show in which girls had discussed cutting themselves as a release, a way to relieve depression. "I was so numb," she said. "I just wanted to feel something — anything." So she took a knife from the kitchen and cut deeply into her left arm.
If Lily had a hard time figuring out what was behind such dark emotions, she was in good company. When a psychoanalyst named Adolph Stern coined the term borderline in the 1930s, borderline patients were said to be those between Freud's two big clusters: psychosis and neurosis. Borderlines, Stern wrote rather poetically, exhibit "psychic bleeding — paralysis in the face of crises." Later, in the 1940s, Dr. Helene Deutsch said borderlines experience "inner emptiness, which the patient seeks to remedy by attaching himself or herself to one after another social or religious group." By 1968, when Basic Books published the groundbreaking monograph The Borderline Syndrome, the No. 1 characteristic of borderline patients was said to be, simply, anger.
Eventually, borderlines became pretty much anything a therapist said they were. Says Dr. Kenneth Duckworth, medical director of the National Alliance on Mental Illness: "If you hated the patient — if the patient was pissing you off — you would bandy this term about: 'Oh, you're just a borderline.' It was a diagnosis that was a wastebasket of hostility."
It was Linehan who changed all that. In the early 1990s, she became the first researcher to conduct a randomized study on the treatment of borderline personality disorder. The trial — which showed that a treatment she created called "dialectical behavior therapy" significantly reduced borderlines' tendency to hurt themselves as well as the number of days they spent as inpatients — astonished a field that had come to see borderlines as hopeless.
Dialectical behavior therapy is so named because at its heart lies the requirement that both patients and therapists find synthesis in various contradictions, or dialectics. For instance, therapists must accept patients just as they are (angry, confrontational, hurting) within the context of trying to teach them how to change. Patients must end the borderline propensity for black-and-white thinking, while realizing that some behaviors are right and some are simply wrong. "The patient's first dilemma," Linehan wrote in her 558-page masterwork, 1993's Cognitive-Behavioral Treatment of Borderline Personality Disorder, "has to do with whom to blame for her predicament. Is she evil, the cause of her own troubles? Or, are other people in the environment or fate to blame? ... Is the patient really vulnerable and unable to control her own behavior ...? Or is she bad, able to control her reactions but unwilling to do so ...? What the borderline individual seems unable to do is to hold both of these contradictory positions in mind."
Linehan's achievement was to realize that borderlines are, in fact, on the border between various dualities — dualities that they have to learn to accept and reconcile in order to change their lives. That's easy to say but seems impossible to do — until you see it work.
A Life Redeemed
After she cut herself, Lily was horrified. In a panic, she called her father, who took her to the hospital. When she was released, she and her parents redoubled their efforts to find her good psychiatric treatment. Through a friend at the University of Washington, they heard about Linehan and contacted her Behavioral Research & Therapy Clinics, which are housed in a homey little annex on the UW campus, where you might find little foil-wrapped chocolates next to the coffee and tea.
Linehan, who grew up in Tulsa, Okla., and spent several years as a nun before becoming a psychologist, embodies several dialectical contradictions: a nun who has never lived in a convent; a careful scientist whose most engaging feature is her wry irreverence; a 65-year-old who has a maternal steeliness but was never a mother. It doesn't pay to underestimate Marsha Linehan. In Cognitive-Behavioral Therapy for Borderline Personality Disorder, she writes, "If the patient says, 'I am going to kill myself,' the therapist might reply, 'I thought you agreed not to drop out of therapy.' "
In one intense session a few years ago, a patient told Linehan that her work stress was going to lead her to suicide. The patient said Linehan could never understand this stress because she was a successful psychologist. Suicidal borderline patients often confront and alienate therapists in this fashion; for many years, this kind of confrontation was seen as a defining characteristic of the disorder. Linehan believes that borderlines are hurting, not manipulating, but that doesn't mean she indulges them. In this particular confrontation, Linehan responded, "I do understand. I live with a similar amount of stress ... You can just imagine how stressful it is for me to have a patient constantly threatening to kill herself. Both of us have to worry about being fired!"
Such in-your-face tactics were highly controversial when Linehan started out. Other mental-health professionals accused her in public meetings of being heartless, even unethical. But her therapy has saved so many lives and worked so well in randomized trials that few criticize her today. For Lily, who calls Linehan's therapy "Zen philosophy meets tough love," Linehan was the first therapist to understand that managing Lily's illness would require Lily to take a new kind of responsibility — a willingness to grow the emotional skin she never had.
In the beginning, Lily resisted Linehan's assistance. She felt no one could truly understand the depths of her pain. But Linehan was the first therapist who responded to Lily with more than just endless psychoanalysis and pills. Instead, Linehan taught her practical methods of getting by day-to-day. Once, just after she started with Linehan, Lily locked herself in her parents' bathroom and swallowed six or seven antidepressants in a half-hearted suicide attempt. Her father broke the door down; her mother called the police. Lily never lost consciousness, but the cops said she had to go to the hospital anyway. Linehan advised Lily's parents not to accompany her. She also told them they needed to get Lily to work the next day. Lily learned that she wouldn't be cosseted.
Linehan also taught Lily various skills to regulate her emotions. Among the most important is one Linehan calls the "wise mind" — a kind of calm, Zen state that Linehan insists even the most debilitated patients can achieve. "Generally," she writes, "I have patients follow their breath ... and try to let their focus settle into their physical center, at the bottom of their inhalation. That very centered point is wise mind." Lily remembers this sensation clearly; she came to feel that her dark moods had a physical location in her body — her solar plexus — and when she focused on it, she could deactivate a destructive emotion.
Another skill Linehan taught Lily (and many others, via a popular DVD called Opposite Action) was an anti-anger technique for social situations: "Don't make the situation worse," Linehan counsels on the DVD. "And if possible, be a little tiny bit on the kind side. O.K.?"
If some of this sounds like advice you heard in kindergarten, it should. Remember that borderlines have never learned to regulate their emotions. It's important to note that Linehan doesn't just practice tough love with her patients; she also tells them she knows they are hurting and doing the best they can. She emphasizes that she believes in them even though many therapists have tossed them aside. "Clients cannot fail," she says. "But both treatment and a therapist can fail." Both compassion and irreverence, both validation and tough love — these are the dialectics at the heart of Linehan's approach.
One criticism of Linehan's Zen-derived method is that for some patients, it seems too foreign, too removed from Western experience. Linehan knows her therapy works for most people, but that doesn't mean she's unwilling to list its faults. "It takes too long. There are too many components. It takes too much training for therapists," she says.
Such shortcomings have not dissuaded other therapists from learning Linehan's techniques. Some 10,000 of them have been trained in dialectical behavior therapy, and Linehan, to her dismay, has become something of a cult figure. "Cults in psychology hurt patients," she says. "People should try whatever works, not my therapy because it has my name on it."
Lily, for one, is glad that it's the therapy she did try. One of her favorite films used to be James Mangold's 1999 adaptation of Girl, Interrupted, in which Winona Ryder plays a real-life borderline author. When Ryder's character learns she has received a diagnosis of borderline personality disorder, she indignantly asks, "Borderline between what and what?" It's a question that weighed on Lily for years and one that many of us may start asking if borderline diagnoses continue to increase. But today Lily is able to laugh about the film because she knows, finally, that the answer doesn't really matter. The key is not defining that uncertain borderline but learning to be happy there.
-
Find this article at:
http://www.time.com/time/magazine/article/0,9171,1870491,00.html
-
------------
"Study may cast light on mental illnesses: 'Default system' of brain measured"
By Carey Goldberg, Boston Globe Staff, January 20, 2009
You're sitting at a dull meeting and your attention drifts. You're waiting in a check-out line, thinking of nothing in particular. You're lying in bed, having just turned off the television. At such times, your conscious mind is on "idle," but your brain is not.
In such situations, the brain's "default system" takes over, a pattern of spontaneous activity that is fast becoming one of the hottest areas in neuroscience research, one that may cast light on mental illness.
Yesterday, researchers from the Massachusetts Institute of Technology, Harvard, and elsewhere reported that the brain's default functions look strikingly hyperactive in people with schizophrenia and their relatives. And the more overactive the default system is, they found, the worse the symptoms tend to be.
The findings are so strong that they raise hopes that brain scans of the default network could be used to diagnose schizophrenia before its symptoms appear, or predict how patients will respond to various treatments, researchers John Gabrieli and Susan Whitfield-Gabrieli said.
"The really exciting thing is that, probably in a year or two, for many, many diseases we'll have a huge amount of evidence about what the situation is in that disease for the default system," said Gabrieli, a professor at MIT's McGovern Institute for Brain Research.
It is already clear that various diseases affect the default system differently, he said. In autism, for example, it tends to be underactive, and in Alzheimer's, part of it seems to go dark.
For years, most neuroscientists paid little attention to what the brain was doing when on idle. But about a decade ago, researchers began to turn their attention to it.
They discovered "a very unique signature" of the brain when the mind wanders, said Marcus Raichle of Washington University in St. Louis, a neuroscientist who pioneered work on the default network. The system they found is "probably key to very core functions of how the brain operates," he said.
Their findings, Raichle said, fit in with the established idea that "the brain is always doing its thing - there is no such thing as a resting state" - which helps explain why it uses 20 percent of the body's energy. They also opened a new vista for research into brain diseases.
The Harvard-MIT paper, published yesterday in the Proceedings of the National Academy of Sciences, found that the default network in schizophrenics was hyperactive when they were at rest, and, importantly, did not ratchet down when they were asked to perform a memory test. Normally, when a subject must perform a task, the activity of the default network diminishes.
The default network findings suggest, Whitfield-Gabrieli said, that schizophrenia involves an inability for a patient's brain "to allocate resources away from their internal thoughts and feelings and toward the external world."
Gabrieli speculated that a hyperactive default network might also help fuel paranoia, by leading patients to interpret external events as being about them: thinking the television is speaking directly to them, for example.
Randy Buckner, a Harvard neuroscientist who studies the default system, said in an e-mail: "This important study suggests how a breakdown in communication between brain systems might cause the cognitive disturbances we see in schizophrenia."
"It is particularly intriguing that the default network is disrupted in schizophrenia, a disorder where the normal boundary between one's own internal thoughts and the outside world is blurred," he wrote.
It is clear that the default network becomes more active when people are thinking about themselves, whether remembering events in their lives or planning an activity.
What remains to be determined, Buckner wrote in a review paper last year, is whether the network's activity represents these self-oriented thoughts or whether its function is, rather, to act as a kind of sentinel monitoring the outside world when a person's thoughts turn inward.
Researchers say a great deal of work on the default network remains to be done, but fortunately, many studies are available for data-mining: Any experiment that looked at the brain's reaction to a task can also be used to examine what the brain was doing when there was no task at hand.
"It's like flipping the contrast," Whitfield-Gabrieli said.
-
Carey Goldberg can be reached at goldberg@globe.com
-
www.boston.com/news/local/massachusetts/articles/2009/01/20/study_may_cast_light_on_mental_illnesses/
-
www.boston.com/news/local/massachusetts/articles/2009/01/20/study_may_cast_light_on_mental_illnesses?mode=PF
-
------------
"Kids' mental ills, drug abuse costly"
By Reuters, February 14, 2009
WASHINGTON - Mental illness, substance abuse, and behavioral problems among children and young adults cost the United States $247 billion a year in treatment and lost productivity alone, an expert panel said yesterday.
The panel set up by the National Research Council and Institute of Medicine that advises policy makers urged the White House to set prevention goals and coordinate government action.
The panel looked at the financial toll from depression, anxiety disorders, and schizophrenia, as well as drug and alcohol abuse and behavioral problems by people up to age 24.
While some school-based programs have been effective, federal leadership has been lacking, the panel said.
------------
AP IMPACT: "Mentally ill a threat in nursing homes"
By CARLA K. JOHNSON, AP Medical Writer Carla K. Johnson, Ap Medical Writer
March 22, 2009
CHICAGO – Ivory Jackson had Alzheimer's, but that wasn't what killed him. At 77, he was smashed in the face with a clock radio as he lay in his nursing home bed.
Jackson's roommate — a mentally ill man nearly 30 years younger — was arrested and charged with the killing. Police found him sitting next to the nurse's station, blood on his hands, clothes and shoes. Inside their room, the ceiling was spattered with blood.
"Why didn't they do what they needed to do to protect my dad?" wondered Jackson's stepson, Russell Smith.
Over the past several years, nursing homes have become dumping grounds for young and middle-age people with mental illness, according to Associated Press interviews and an analysis of data from all 50 states. And that has proved a prescription for violence, as Jackson's case and others across the country illustrate.
Younger, stronger residents with schizophrenia, depression or bipolar disorder are living beside frail senior citizens, and sometimes taking their rage out on them.
"Sadly, we're seeing the tragic results of the failure of federal and state governments to provide appropriate treatment and housing for those with mental illnesses and to provide a safe environment for the frail elderly," said Janet Wells, director of public policy for the National Citizens' Coalition for Nursing Home Reform.
Numbers obtained through the Freedom of Information Act and prepared exclusively for the AP by the Centers for Medicare and Medicaid Services show nearly 125,000 young and middle-aged adults with serious mental illness lived in U.S. nursing homes last year.
That was a 41 percent increase from 2002, when nursing homes housed nearly 89,000 mentally ill people ages 22 to 64. Most states saw increases, with Utah, Nevada, Missouri, Alabama and Texas showing the steepest climbs.
Younger mentally ill people now make up more than 9 percent of the nation's nearly 1.4 million nursing home residents, up from 6 percent in 2002.
Several forces are behind the trend, among them: the closing of state mental institutions and a shortage of hospital psychiatric beds. Also, nursing homes have beds to fill because today's elderly are healthier than the generation before them and are more independent and more likely to stay in their homes.
No government agency keeps count of killings or serious assaults committed by the mentally ill against the elderly in nursing homes. But a number of tragic cases have occurred:
• In 2003, a 23-year-old woman in Connecticut was charged with starting a fire that killed 16 fellow patients at her Hartford nursing home. A court guardian said Leslie Andino suffered from multiple sclerosis, dementia and depression. She was found incompetent to stand trial and committed to a mental institution.
• In 2006, 77-year-old Norbert Konwin died at a South Toledo, Ohio, nursing home 10 days after authorities said his 62-year-old roommate beat him with a bathroom towel bar. Sharon John Hawkins was found incompetent to stand trial.
• In January, a 21-year-old man diagnosed with bipolar disorder with aggression was charged with raping a 69-year-old fellow patient at their nursing home in Elgin, near Chicago. A state review found that Christopher Shelton was admitted to the nursing home despite a history of violence and was left unsupervised even after he told staff he was sexually frustrated.
Jackson's roommate was 50 and had a history of aggression and "altered mental status," according to the state nursing home inspector's report. Solomon Owasanoye wandered the streets before he came to All Faith Pavilion, a Chicago nursing home, and he yelled, screamed and kicked doors after he got there.
On May 30, 2008, he allegedly picked up a clock radio, apparently while Jackson slept, and beat him into a coma. Exactly what set him off is unclear. Jackson died of his injuries less than a month later. Owasanoye pleaded not guilty to first-degree murder, and after a psychiatric review was ruled unfit to stand trial. He now lives in a state mental hospital.
All Faith Pavilion co-owner Brian Levinson said his staff is trained to deal with aggressive behavior, and he disputed state findings that Owasanoye had a history of aggression. The for-profit nursing home was fined $32,500 for failing to prevent the assault.
Under federal law, nursing homes are barred from admitting a mentally ill patient unless the state has determined that the person needs the high level of care a nursing home can provide. States are responsible for doing the screening. Also, federal law guarantees nursing home residents the right to be free from physical abuse.
Families have sued in hopes of forcing states to change their practices and pressuring nursing homes to prevent assaults. Advocates say many mentally ill people in nursing homes could live in apartments if they got help taking their medication and managing their lives.
The problem has its roots in the 1960s, when deplorable conditions, improved drug treatments and civil rights lawsuits led officials to close many state mental hospitals. As a result, some states have come to rely largely on nursing homes to care for mentally ill people of all ages.
Also, mixing the mentally ill with the elderly makes economic sense for states. As long as a nursing home's mentally ill population stays under 50 percent, the federal government will help pay for the residents' care under Medicaid. Otherwise, the home is classified a mental institution, and the government won't pay.
In Missouri, more than 4,400 younger mentally ill people are living in nursing homes, in part because of a state program that helps the elderly stay in their own homes longer.
Nursing homes "are looking at 60 to 70 percent occupancy, and the statistics tell us they've got to be in the 90s to operate successfully," said Carol Scott, the state long-term care ombudsman for 20 years. "They're going to take anybody they can."
Gaps in staff training leave the homes inept at handling the delusions and aggression of the mentally ill, said Becky Kurtz, the state long-term care ombudsman in Georgia, where nearly 3,300 younger mentally ill people live in nursing homes.
"Often they'll say, 'I hate it there. I'm angry. I don't want to be there.' Sometimes the behavioral issues are the result of being ticked off you're in a nursing home," Kurtz said.
Pat Willis of the Center for Prevention of Abuse said she has seen elderly residents terrified by younger, mentally ill residents who scream and yell, day and night. "The senior residents are afraid," Willis said. "They would prefer to sit in their rooms now and keep the doors shut."
Nursing home operators say protections against frivolous transfer or discharge keep the homes from throwing out some mentally ill residents.
"Many times, the nursing home's only option becomes dialing 911," said Lauren Shaham, a spokeswoman for the American Association of Homes and Services for the Aging.
------------
"Firms tied to some MDs who set policy: Treatment advice focuses on drugs, researchers find"
By Carey Goldberg, Boston Globe Staff, April 2, 2009
Virtually all the psychiatrists who wrote the latest clinical guidelines for how to treat depression, bipolar disorder, and schizophrenia had financial ties to drug companies, according to preliminary findings by Boston-based researchers.
Their study is the first to examine potential conflicts of interest in the American Psychiatric Association panels that write the treatment guidelines widely used by practitioners, the paper's authors said.
The guidelines focus heavily on medications and give relatively little attention to nondrug treatments and how and when to phase out drugs prescribed for mentally ill patients, the authors wrote. They said three common diagnoses generate some $25 billion in drug sales per year.
"Most patients assume that when they're prescribed a drug, the decision is made on the basis of an objective review of the scientific evidence," said the paper's lead author, Lisa Cosgrove of the University of Massachusetts at Boston. "However, our study raises the question: Is that decision based in science, or is there a financial incentive behind it? This is an important question because the lack of biological tests for mental disorders renders psychiatry especially vulnerable to industry influence."
The psychiatric association re sponded that its guidelines, which sum up research and real-world experiences with treatments, go through a long and elaborate vetting process and that people who get significant portions of their income from drug companies are excluded from the guideline panels.
"We work very hard to ensure that the guidelines that we develop and publish are free of bias to the greatest possible extent," said Dr. John S. McIntyre, chairman of the guideline steering committee.
The study, scheduled to be published online this month in the journal Psychotherapy and Psychosomatics, found that among 20 authors of the guidelines, 18 had at least one financial tie to drug companies. It did not name names or specify sums, but found that 12 guideline authors had ties in at least three categories, such as consulting, research grants, speaking fees, or stock ownership.
To find financial ties, Cosgrove and her colleagues, who included Sheldon Krimsky of Tufts University and Dr. Harold Bursztajn of Harvard Medical School, searched publicly accessible databases such as Medline and the records of the federal patent office.
Dr. Roy Perlis, listed as a consultant on the bipolar guidelines, works in psychiatric genetics at Massachusetts General Hospital. In published papers - including one that examined financial conflicts of interest in clinical trials of psychiatric medications - he disclosed having received consultant or speaker's fees from five major drug companies: AstraZeneca, Bristol-Myers Squibb, Eli Lilly, GlaxoSmith Kline, and Pfizer.
But Perlis noted that the guidelines for bipolar disorder make two main points, neither of which benefit drug companies: that lithium, which has long been available as an inexpensive generic drug, is still the "gold-standard treatment" and "that certain kinds of talk therapy are a very important part of treatment."
"My job is to find better treatments for my patients. These are awful illnesses. People really suffer," he said. "And the people who are most responsible for developing new treatments right now are the pharmaceutical companies. What is being lost in all this is that if I didn't work with them, I couldn't do my job as a scientist - the part of my job that says we have people who are suffering that need new treatments."
The pharmaceutical industry defends its practice of paying "thought leaders" in various specialties to lend their expertise to drug development and marketing, saying that their input benefits both colleagues and patients and that they must be paid for their work.
But there is a growing backlash against conflicts of interest in medicine. A posse of those pushing for change in the medical culture is centered in Boston and includes Drs. Marcia Angell and Jerome Kassirer, former editors of the New England Journal of Medicine, and researchers such as Cosgrove and Krimsky. These critics contend that financial ties introduce the potential for bias, and at the very least, all such ties must be disclosed.
"What we're saying," said Krimsky, is that guideline writers "should be totally transparent about their relationships with the drug companies so people reading a guideline might ratchet up the skepticism they might have about the use of drugs as the first line of therapy."
This week in the Journal of the American Medical Association, a group of influential medical leaders went further, calling on medical specialty groups to adopt tough policies against industry influence, including appointing "only individuals who have no ties to industry" to committees writing treatment guidelines. Among the leaders, who specified they were not acting as representatives of their organizations, was the medical director and CEO of the psychiatric association.
The psychiatric association now requires guideline writers to publish any financial ties along with the guidelines they work on, but at the time the current guidelines for depression, bipolar disorder, and schizophrenia were published in 2004 and 2005, no such disclosures were required.
McIntyre, of the psychiatric association, said the steering committee that oversees the guideline-creation process has always screened proposed members of the groups that work on each set of guidelines for potentially troubling ties, including spouses who work for drug companies. The idea, he said, is to avoid people who get more than roughly 5 percent to 15 percent of their income from pharmaceutical firms, especially when from one particular company.
It would be a mistake to disqualify everyone with drug-company ties, he said, because it would mean losing valuable expertise in research that must be evaluated, but the association is considering whether to set a limit on committee members' industry income and research support.
The guidelines - the psychiatric association has produced 16 - also go out to hundreds of psychiatrists and others for comment and review, McIntyre said. "When you subject a document to that kind of review, by a large number of people, a single voice that might unwittingly be biased gets diluted," he said.
The new paper found that all of the authors of the schizophrenia and bipolar guidelines had relationships with the drug industry, and 60 percent of the authors on depression did. More than three-quarters received research funding from drug companies, and more than one-third served on the speakers' bureaus of drug companies.
In an editorial, this month's American Journal of Psychiatry singles out speakers' bureaus as the clearest example of conflict of interest, noting that they supply prominent psychiatrists "to deliver company-approved presentations that market their drugs to their clinical colleagues in the guise of medical education."
------------
-

-
"Should I?: One woman's struggle with bipolar disorder - and the question of whether to become a mother."
By Marya Hornbacher, The Boston Globe Online, IDEAS, Sunday, April 5, 2009
MY HUSBAND AND I were weeks away from flying to Haiti to pick up our newly adopted baby. We'd been in the exhausting, exhilarating process of adoption for six months. We had the nursery all set to go. Our parents were turning cartwheels with excitement about the new grandchild. In our approved application, we had more letters of recommendation than I can count - from friends, employers, family members, and one glowing letter of recommendation from my psychiatrist.
Then I got sick.
It was February? Maybe? Time slips and slides when mental illness sets in. In any case it was winter. I was lying on my side in the psych ward, facing the flat white wall. Tears leaking into my ears. I wouldn't say I was sad. Depression's not like sadness. More like death. Empty and silent and dull. Behind me, at the side of the bed, sat my mother and stepfather. My husband was sitting beside me on the bed.
"I can't," I whispered.
"What?" they said, leaning closer.
"I can't do it," I said. "We can't get the baby."
I was so sure, at that moment, that I was making the right decision. I believed, for that one life-changing instant, that I truly wasn't capable of raising a child, that any child would be better off without me as its mother. Lying there in a hospital bed, the idea of taking care of something so fragile as a child, when I couldn't even take care of myself, made my head spin. So I said no.
It was obvious: I wasn't up for that kind of responsibility. Wasn't reliable enough, was maybe too volatile to be trusted. Yes, maybe I had wanted it, but what about the best interest of the child? That day, I, like a whole lot of people, believed that mental illness really did disqualify me as a parent.
Now, I'm not so sure.
I have bipolar disorder. Bipolar is a mood disorder, a brain disease that, when uncontrolled, causes the patient to vacillate between manic and depressive episodes, with periods of stability in between. There are about 15 million adults in the United States with bipolar.
Bipolar has taken me on a wild and terrifying ride. For 20-odd years, my moods swung from uncontrolled manias that sometimes veered into psychosis to depressions that plummeted me into catatonia, the highs and lows cycling so rapidly I couldn't keep up. Like a great many people with mental illness, I resisted my diagnosis - who wants to believe they're mentally ill? - and with it resisted the medication that would make it manageable. And like about half of people with bipolar, I struggled with substance abuse for years. For someone with a mental illness, drinking and doing drugs is like pouring gas on an already smoldering fire.
My life for years was a rollercoaster - professional success, personal disaster, mania, depression, hospitalization after hospitalization. There is no question that, during those years, I should not have had children.
After running from the reality of my situation for far too long, losing nearly everything and everyone I cared about, trying six ways from Sunday to tell myself I could get a handle on it if I just pulled myself up by my bootstraps - I finally gave in and got the treatment I desperately needed.
And everything changed. I realized that, in fact, they weren't kidding - mental illness really is treatable. It's a chronic disease, like diabetes, and managing it takes effort, but it can be done - and millions of people do it every day. I got my illness under control by treating it aggressively with medication, therapies, changes to my lifestyle, and a host of little tricks of the trade that keep me stable, healthy, and highly functional.
This means that, in most ways, I've left behind the chaos of my earlier life and joined the ranks of "normal." People who manage their mental illness are all around you, and you probably don't know it, because they look and act just like you. They go to work, buy groceries, drink lattes, and have kids. That's what's funny - I imagine a whole lot of people would think I'd make a great mom, right up till the moment they learned I have a mental illness.
. . .
I recently wrote a memoir on living with bipolar disorder. I was signing books at a lecture. A woman came up to the table and, after saying all sorts of earnest things about how important it was to break down stigma, broaden understanding, and so forth, she suddenly gasped.
"Is that a wedding ring on your hand?" she asked. I looked down and indeed it was a wedding ring, so I said, "Yes."
"You're married?"
I said that I was.
"My God!" she said. "He must be an amazing man!"
Um? On and off, more or less.
"Well," she said, looking alarmed. "But you don't have children, do you? I mean, I would think you wouldn't want to pass on your genes."
I froze.
"Right," I said, and smiled, and signed her book, and she went away.
Apparently I hadn't quite made my point. Because after 45 minutes of going on about the facts that mental illness is highly treatable, that one can live and live well when one has it, and that my life as a mentally ill person is really quite average, she'd come away with: mentally ill people are so warped that it's a miracle anyone can stand being married to them, let alone allow them to inflict themselves on a baby.
The durability of the stigma surrounding mental illness is astounding. People still carry in their minds the image of the raving lunatic. The very fact that the question of whether mentally ill people should have children is a subject of debate points up a few assumptions that are wildly off base - that people with mental illness are all the same; that they're by definition unstable; and that people without mental illness are in a position to arbitrate the lives of people about whom they know precious little.
Mentally ill people exist on a wide spectrum - of severity of illness, of the extent to which it is controlled, of personality, of potential as parents. Some of us would be, and are, very good at parenting, some not so much. The decision to raise children is highly personal, and requires a clear understanding of who we are, what we're capable of, what we have to offer, and what we'll have to watch out for. That's true of anyone, mentally ill or not.
It's true that there are plenty of people with mental illness who just aren't equipped for child rearing. Not every mentally ill person manages their illness; some refuse the medication that would get it under control, some can't afford it or the insurance that would cover it, others have symptoms that resist treatment.
When people with uncontrolled mental illness have kids, those kids do feel the effects, and it's a serious struggle for both parent and child. But unless we want to skate dangerously close to the suggestion that those people should not be "allowed" to have children - a suggestion that leads ultimately to an argument for eugenics - "we" are not in a position to say that they can't have kids.
I would venture to say that many people start having children without deeply thinking it through, and without being particularly well-prepared. Who allows them to do this? Well, that's not really the question. We sigh and say, God, there should really be a test. But we're joking.
No one expects parents to be perfect. All parents have emotional lives, have flaws, have breaking points, have bad days, bad weeks, sometimes a bad year here and there. Parents work too much or lose their jobs. Parents without mental illness go through deep emotional struggles of their own, parents wish they'd never had kids, parents are occasionally terrible role models. Parents are human like anyone else.
And many people with mental illness - myself included - are as functional, and forgivably flawed, as the average parent. Yes, my bipolar is a significant facet of my day-to-day experience, but it doesn't stop me - doesn't stop me from working, loving, being part of a community and a family - and it would no more stop me from parenting well than diabetes would.
. . .
My father had severe depression, which wasn't treated until I was in my 20s. Growing up with it affected me. It was frightening to watch, but it wasn't nearly as important as the fact that he took me to baseball games, came to every soccer game and junior high musical, crowed over every A, instilled me with a powerhouse work ethic, showered me with books, told me I could be anything I wanted to be, and was always, always there.
The children we were planning to adopt didn't have that love in their life, and we wanted to give it to them. We wanted to read to them, and wipe their noses when they were sick, and let them draw on the walls, and sing them to sleep. There are millions of children all over the world who desperately need that kind of family, that safe place to be, that guidance, that enveloping love. And I decided, in a moment of radical fear and self-doubt, that I didn't have it to give.
I sometimes have this dream where I am holding a thing, and then it floats away, and I get this weird weightless ache in my arms. Then I wake up and listen to the silence. It is the noisy silence of the ghost of the 5-year-old I chose not to raise. Is anyone raising her?
You often hear people with mental illness who have children described as "selfish." There's the perception that someone like me would have kids only to serve my own needs. But maybe the decision I made was the selfish one. My arms are empty. And my burden is very light.
-
Marya Hornbacher is the author of three books, most recently "Madness: A Bipolar Life," now available in paperback.
-
------------
-

-
"The other kind of smart: Is it time for schools to try to boost kids' emotional intelligence?"
By Drake Bennett, The Boston Globe Online, IDEAS, Sunday, April 5, 2009
FOR MOST OF us, what we were taught in school and what we remember from our school years are two different things. We sat through uncountable hours of lessons about denominators and organelles, about precipitates and dangling participles, about Boo Radley and Shays' Rebellion, and yet the memories that sneak up on us today are more likely to be the humiliations suffered on the school bus or the awkward moments from a pubertal romance, the triumph of a deftly parried insult or the sheltering solidarity we felt in a now long-dispersed clique.
Much of what we learn about social life, in other words, we learn in school. The learning process is a fumbling and painful one, administered not by teachers but through schoolyard intrigues and emotional outbursts. And in this part of our education, we are largely on our own. While some people - Franklin Delano Roosevelt was one, Ronald Reagan another - seem born with a gift for emotional perception, the rest of us muddle through as we can. School is set up for one kind of learning, but when it comes to emotional matters, the assumption has always been that these are instincts we have to develop for ourselves.
Today, however, a number of educators and psychologists are arguing that, actually, we don't. What they call "social and emotional knowledge" - the ability to read other people, manage our own emotions, and thereby master social situations - doesn't have to be imparted solely through the cut and thrust of lived life. It can be taught, they say, just like trigonometry or French grammar. Psychologists are designing curricula that aim, step by step, to build up students' emotional knowledge: a typical teaching unit might include a role-playing exercise, or a set of diagrams breaking down the components of different facial expressions, or, in older children, a discussion of the subtle differences between disgust and contempt.
And while the basic idea that school should help refine social skills is not a new one, the proponents of social and emotional literacy programs are armed and emboldened by promising new findings that suggest just how teachable these skills are. With a little training, studies show, grade-schoolers can dramatically improve how accurately they read emotions in others' faces, how well they head off impending tantrums - even how empathetic they are toward classmates.
Education officials are starting to take notice. Around 10 percent of American grade school and high school students now go through some form of social and emotional learning curriculum, according to the Collaborative for Academic, Social, and Emotional Learning (CASEL), a Chicago-based emotional learning research organization. A handful of states have instituted emotional learning guidelines for their public schools - the most comprehensive is Illinois's, which sets "self-management," "social awareness," and "interpersonal skills" benchmarks, among others, for kids at each grade level.
The movement has been fed by a confluence of factors. Parents and school administrators are increasingly worried about the disruptive effects of bullying and other antisocial behaviors in schools. At the same time, cognitive scientists are emphasizing the vital role emotions play in rational thought.
Supporters point to a growing collection of studies showing the benefits of emotional learning programs in everything from test scores to lowered anxiety levels and rates of drug use. But the ultimate goal is something larger: a redefinition of what school is meant to teach, and what sort of knowledge we value. What emotional literacy campaigners are arguing is that the problems of the American school system won't be solved by getting kids reading sooner or ensuring that they can find Alaska on a map - they need to better understand what drives them and others.
"This is not meant to be part of the school mental health plan, but part of the regular instructional plan," says Mary Utne O'Brien, a research professor at the University of Illinois at Chicago and an executive at CASEL. "It's about more than making school nice; it's specific skills, just like what you're doing in language or math."
The champions of emotional learning claim an intellectual pedigree stretching back to Aristotle, who described emotional control and understanding as vital virtues. Writing in the early 20th century, the philosopher and influential education reformer John Dewey fleshed out this idea, insisting that schools should impart not just information but habits of mind that would ensure that graduates were active participants in a democratic society. Educational reformers in the intervening decades have echoed Dewey's arguments.
Still, these ideas have had a hard time finding purchase in the traditional "reading, writing, and arithmetic" curriculum, especially as standardized tests on traditional topics have come to determine more and more of how students and their schools are judged.
Today's emotional education movement, however, is energized by something new: a surge of studies suggesting that "softer" knowledge like social and emotional skills can be analyzed and taught in the same way that math and critical thinking can be.
The emotional knowledge research field arose in the early 1990s with the work of the psychologists John Mayer, of the University of New Hampshire, and Peter Salovey of Yale. Mayer and Salovey weren't interested in emotional knowledge per se, but emotional intelligence: people's ability to process new emotional information (a sort of emotional IQ). But, according to Mayer, their interest grew out of earlier research exposing some of the mechanics by which emotions guide us and, at times, give us away - work by the neurologist Antonio Damasio, for example, showed how people rendered emotionless by brain damage became not more but less rational in many ways. Also influential was psychologist Paul Ekman, who developed an exhaustive taxonomy of what he called "micro-expressions," tiny, inadvertent facial movements that betray our true emotions. (The current TV crime drama "Lie to Me" is inspired by Ekman's work.)
In Ekman's work in particular, seemingly innate social skills were being broken down into the kind of units that could be studied, and taught - Ekman began offering courses in how to spot and interpret micro-expressions.
What really transformed the field, however, was the 1995 publication of the runaway bestseller "Emotional Intelligence," by the psychologist and journalist Daniel Goleman. In the book, Goleman drew on Mayer and Salovey's work but also made some sweeping arguments of his own. The book was written for a popular audience, and emotional intelligence researchers are careful to distance themselves from some of its more dramatic claims. But its popularity fueled interest among educators, and the sometimes seat-of-the-pants emotional education efforts they embarked on provided ample research fodder for curious psychologists.
In recent years, the results have started to come in, and they suggest that emotional knowledge can indeed be learned in the classroom. Emory University psychologist Stephen Nowicki has found that interventions can teach kids to read faces better. Mark Greenberg of Penn State has found that emotional learning classes can make kids better at controlling themselves when upset. Researchers looking at a curriculum called the Resolving Conflict Creatively Program found that such classes also made children less likely to falsely misread intent - in particular less likely to assume hostility in ambiguous social situations.
"The extent to which this is now research-based is new," says Larry Dieringer, the executive director of the Educators for Social Responsibility, a Cambridge-based education-reform research organization. "The accumulation of evidence has been both basic research about brain development and evidence that comes from the evaluation of social and emotional programs."
Among the most highly regarded of the curricula that both fed and fed off that research is one created by Marc Brackett, the deputy director of the Yale University's health, emotion and behavior laboratory. His program is dubbed RULER (for Recognizing, Understanding, Labeling, Expressing, and Regulating emotions) and Brackett has trained more than 25,000 teachers in it.
"People are just not exposed to this information because it hasn't been valued in our society," Brackett argues. "I can show that people can become better at it."
The RULER curriculum is tailored to different age groups, but in general it involves dozens of sessions: workshops in which students discuss feelings they are having or interview each other about their emotions, role-playing exercises in which they act out different emotions or are presented with emotionally charged situations, then have to work through how to defuse them. There is an emphasis on learning a richer vocabulary to describe emotions, the idea being that students better able to express how they feel will be both more conscious of their feelings and less likely to be misunderstood by others. And there are Ekman-like courses in basic facial expression recognition - many kids, Brackett says, confuse surprise and fear.
One of the central tools of Brackett's system is something he calls the "mood meter," a 2-by-2 chart on which kids can plot their subjective state along with their energy level. Brackett argues that doing so allows kids to better understand what they're feeling and even why. High energy and positive is excited, low energy and positive is relaxed; low energy and negative is sad or depressed, high energy and negative is agitated or angry. A more fine-grained, systematic understanding about what emotions are, Brackett argues, is a key step in learning how to anticipate and control them.
The Obama administration has made clear that it plans to use the tens of billions of stimulus dollars it is injecting into the nation's schools as leverage to demand reform. Much of the administration's agenda has yet to be spelled out, but there is a sense in the education world that fundamental changes could result. And while the administration has yet to mention emotional learning, champions of the idea have taken heart at smaller signals of support: California congressman George Miller, for example, chair of the House Education Committee, has expressed interest in the idea of using federal money to help expand emotional learning programs.
With the administration's much-touted affection for data-driven decision-making, emotional learning supporters believe their growing bundle of research results will only help their cause. Several recent studies have linked social and emotional learning programs to a variety of positive outcomes: better grades, fewer fights, less drug use, and the ability to form more lasting personal relationships.
Still, there are psychologists who argue that it's still very early - after all, general intelligence has been a topic of debate for more than a century - and that teaching emotional intelligence comes with its own risks. In "What We Know About Emotional Intelligence," a book due out this month, the psychologists Moshe Zeidner, Gerald Matthews, and Richard Roberts point out that there's little research demonstrating how emotional learning programs work. And since many programs combine emotional learning with things like antibullying and antiviolence workshops, it's hard to tease out the effect of the emotional curriculum alone.
These critics also raise the question of whether a classroom full of emotionally aware kids might also be a class of adroit emotional intriguers. "If you know how to understand and manipulate other people's emotions, it can turn into something Machiavellian," says Zeidner, director of the center for interdisciplinary research on emotions at Israel's University of Haifa.
Other critics wonder whether reducing social and emotional life to a series of workshops and tests, where some emotions are right and others wrong, risks creating a sort of emotional conformism, the opposite of the vigorous taste for dissent that John Dewey wanted to inculcate.
Supporters of the programs dismiss these concerns as unfounded - the best programs, they argue, are about perceiving and managing emotions, not stifling them. But at the same time, they point out, uniformity runs both ways. Part of the appeal of emotional learning curricula is that they promise to make up for the fact that some kids come armed with a well-developed social sense and all the benefits it confers, and some do not.
"The 'aha' of this field is that it doesn't have to be the luck of the draw - coming up in a family that has it together or naturally being a people person or a self-aware person," says O'Brien, of CASEL. "It's that you can teach these skills to everyone."
-
Drake Bennett is the staff writer for Ideas. E-mail drbennett@globe.com.
-
------------
"Making sense of autism: A panel of experts shed light on the subject at Berkshire Medical Center"
By Benning W. De La Mater, Berkshire Eagle Staff, Friday, April 17, 2009
PITTSFIELD — One girl had an intense desire to fill small bottles with her feces.
A boy who could solve advanced calculus equations also had a penchant for tying himself to cafeteria chairs.
Another enjoyed debating the origins of Faust yet couldn't hold back expressing negative opinions of others.
These are a few glimpses into the world of autism, and they were provided by a panel of experts Thursday night at Berkshire Medical Center — psychiatrists, psychologists and patients who have spent decades working with the developmental disorder and living it.
Sponsored by Elms College in Chicopee, the discussion drew a capacity crowd to the BMC auditorium — 140 parents, patients, physicians, teachers and child-care professionals all looking to learn more about an affliction that continues to stump society.
Kathleen Dyer, clinical director of the River Street Autism Program outside Hartford, Conn., said there are more questions than answers. But there is hope.
In the early 1970s, "the treatment was to put them in state hospitals and heavily medicate them," Dyer said. "They treated kids with LSD."
Today, the American Pediatric Association has a set of guidelines for screening and diagnosis. The economic stimulus package includes $80 million allocated for autism research.
"And autism treatments are now being legislated to be covered by insurance," Dyer said.
Michael Rice, a psychologist at River Street, called the disorder "baffling."
He said the statistics make it even more daunting. The U.S. Centers for Disease Control and Prevention says the incidence of autism has risen from one in 5,000 in 1970 to one in 150 in 2008.
Is it more prevalent today or are doctors more educated?
"We don't know," Rice said. "Are we doing better with the diagnosis? Yes. There's a real emphasis on early detection."
Symptoms of autism can included a lack of social and verbal skills, an inability to learn simple tasks, and repetitive behaviors. It can range from a child who cannot speak at all to one who is highly skilled in certain areas, like math.
It affects all races and cultures. Rice said doctors are now able to diagnose children as young as 1. The focus of treatment, he said, deals with two areas: Stopping a child's destructive behavior and teaching life skills.
Dr. Richard Sadler, a psychiatrist at River Street, said some medications help certain patients.
"But nothing is a proven fix," he said. "Do meds improve quality of life? Maybe, maybe not."
Dyer urged parents to educate themselves.
"Research the methods that have been suggested," she said. "Get connected with a community of parents and professionals."
It can be maddening, though. With autism awareness on the rise — Google "autism" and you'll get 18 million hits — there seems to be a sea of voices saying different things.
"We need evidence-based research and practices," Dyer said. "Treatment needs to be early and intensive."
John Robison showed the crowd that there is hope. The Amherst resident and author of the best-selling book "Look Me In the Eye" has dealt with Asperger syndrome most of his life.
Kids called him "retard," he dropped out of high school, and yet he had a knack for electronics, which would later help him land a gig designing equipment for Pink Floyd and KISS. He went on to make electronics for Milton Bradley and started a high-end automotive repair business.
He said he always had "social blindness," almost an inability to sense emotions from people around him. A customer who was a psychologist was the first one who told him he might be an "Aspergian."
"From that point on I decided to make myself normal," he said.
He speaks to crowds about autism and encourages patients to seek help, a notion that all the experts agreed with.
"We need comprehensive treatments and more research," Dyer said. "We can't fix everyone, but can bring 90 percent of them to a better place."
-
To reach Benning W. De La Mater: bdelamater@berkshireeagle.com, (413) 496-6243.
-
------------
"Brien Center physician named clinician of the year"
The North Adams Transcript, 4/20/2009
PITTSFIELD -- Richmond resident Jennifer L. Michaels, M.D., a physician with The Brien Center in Pittsfield, has been named 2009 Community Clinician of the Year by her physician peers of the Berkshire County District Medical Society.
The Community Clinician of the Year Award was established in 1998 by the Massachusetts Medical Society to recognize a physician from each of the society's 20 district medical societies who has made significant contributions to his or her patients and the community.
A graduate of the New York University School of Medicine, Michaels is dual board-certified in general psychiatry and addiction psychiatry. She is the medical director for all psychiatric services at The Brien Center, one of Berkshire County's largest providers of community mental health and substance abuse services.
The Brien Center provides comprehensive psychiatric care to over 10,000 Berkshire county residents each year.
Michaels is a national mentor to other psychiatrists through the Substance Abuse and Mental Health Services Administration's Physician Clinical Support System. She is a frequent discussant on National Public Radio, and often speaks at community forums regarding mental health issues.
Michaels is a member of the Co-occurring Center for Excellence for the National Council of Community Behavioral Healthcare, a nonprofit association representing 1,300 organizations providing treatment and rehabilitation to help people recover from mental illnesses and addiction disorders.
Michaels has served as an attending psychiatrist at McLean Hospital in Belmont and as a faculty member at Harvard Medical School.
She is currently an assistant professor at the University of Massachusetts Medical School.
The Brien Center is the primary mental health and substance abuse provider to the region, and is the sole provider for the uninsured and underinsured.
In addition, Brien Center provides specialized elder services, and child and adolescent after-school, outreach, and family stabilization programs.
The organization provides the region's 24/7 Crisis/Emergency Services, which provide mobile outreach assessments in a variety of locations, including the emergency rooms of all three Berkshire hospitals, police stations, schools, etc. Emergency services also include two stabilization programs (adult and child) to serve as an alternative to hospitalization or as a step down from the hospital before the patient is ready to go home.
Brien Center services are open to all segments of the Berkshire County population. More than 10,000 people are served annually at Brien's North, Central, and South County locations. Of the 10,000 served, about 500 are chronically mentally ill; the largest percentage of our outpatient service is for treatment of individuals with anxiety and depression. Three thousand of its clients are children.
------------
"Ashuwillticook event to support mental health education"
North Adams Transcript - 5/5/2009
CHESHIRE -- NAMI, The National Alliance on Mental Illness of Berkshire County will host the fourth annual hometown walk-run-pedal-paddle-hop-skip-or-jump-a-thon from 10 a.m. to 1 p.m., Saturday, May 30, 2009, at the Ashuwillticook Rail Trail, Farnams Crossing, Route 8, in Cheshire. Funds raised will be used to support local mental health education.
To register or obtain a walk brochure, call NAMI-BC at 1 (413) 443-1666. To donate online, visit www.namibc.org.
Whether you walk, run, pedal or paddle, this event will be fun for everyone. You can stretch your legs on the three mile course as you stretch your minds and hearts and help raise awareness about mental illness.
Registration begins at 10 a.m. Honorary champion, Dr. Alex Sabo, the department chair of Psychiatry & Behavioral Health at Berkshire Medical Center, will conduct the ribbon-cutting ceremony to start the walk at 11 a.m. Finish line activities will include an awards ceremony with trophies for the family, team and individual who raises the most money for NAMI, followed by a barbecue lunch and entertainment by Robin O'Herin, blues and gospel singer, and many other surprises.
NAMI, the National Alliance on Mental Illness, is a nonprofit grassroots self-help, support and advocacy organization of consumers, families and friends of people with severe mental illnesses, such as schizophrenia, major depression, bipolar disorder, obsessive-compulsive disorder, and anxiety disorders.
NAMI-BC is dedicated to eradicating the stigma of mental illness and to the improvement of the quality of life of all those whose lives are affected by mental illness in Berkshire County through education, advocacy and support and is a member agency of the Berkshire United Way and Northern Berkshire United Way. For further information about this event and NAMI-BC, contact Bonnie Brace, executive director, at (413) 443-1666 or e-mail namibc@namibc.org.
------------
"Study: Some autistic kids overcome the disorder"
By Lindsey Tanner, Associated Press, May 9, 2009
CHICAGO - A small but provocative study suggests that at least 10 percent of children with autism overcome the disorder by age 9 - most of them after undergoing years of intensive behavioral therapy.
Skeptics question the phenomenon, but University of Connecticut psychology professor Deborah Fein is among those convinced it's real.
She presented research this week at an autism conference in Chicago on 58 children, including 20 who, according to rigorous analysis, got a correct diagnosis but years later were no longer considered autistic.
Among them was Leo Lytel of Washington, D.C., who once made no eye contact, who echoed words said to him and often spun around in circles - all classic autism symptoms. Now he is an articulate, social third-grader. His mother, Jayne Lytel, says his teachers call Leo a leader.
The study, funded by the National Institute of Mental Health, involves children ages 9 to 18.
Geraldine Dawson, chief science officer of the advocacy group Autism Speaks, called Fein's research a breakthrough.
"We're at a very early stage in terms of understanding" the phenomenon, Dawson said.
------------
"Real needs of Asperger's students"
The Berkshire Eagle, Letters, Saturday, May 30, 2009
Brian Sullivan has taken on the case of a teen with Asperger's Syndrome as an example of outrageous demands being made on (Pittsfield) public schools. ("Dracut makes tough jobs even tougher," May 21). If you actually read this decision (spanmass.org), made by a BSEA hearing officer, you will find that the requests for transition services had been made multiple times by the family and ignored by the school. It is more than social skills that this teen needs help with — systematic, step-by-step pragmatic language instruction, development of organizational skills, vocational training, travel instruction, a comprehensive social skills assessment, as well as training in social skills.
All of these could have been accomplished within his IEP while he was a student. The school decided to ignore these needs and get him graduated — focus on MCAS, not on real life.
If you want to be irate, focus on the waste of money and resources needed to work on passing MCAS while education is ignored. This is not an issue that affects only children with disabilities, it affects every child who attends a public school. If you want to help, support the Special Education teachers who generally are under-supported and overburdened with unrealistic expectation from the state and administration level.
If you want to help, ask what they need to accomplish "educating'' a student beyond MCAS. If you really want to help, become a mentor to a teen who is struggling to make sense out of a world that really doesn't care what your grades were. Offer your time, hobby or place of employment to give a student experience in the real world.
People with Asperger's have a great future if their educational needs are addressed. What would the world be without Woody Allen, Bob Dylan, Carl Jong, Oliver Sachs and Bill Gates!
BARBARA COUTURE
Williamstown, Massachusetts
-
www.topix.net/forum/source/berkshire-eagle/TM4G512F8OCMPQO04
-
------------
"'Eco-Therapy' for Environmental Depression: Go Jump Off a Pier"
By BRYAN WALSH Bryan Walsh, TIME via news.yahoo.com - Monday, July 27, 2009
Depressed people often need someone to hug. On occasion, that someone may just be a tree.
A new and growing group of psychologists believes that many of our modern-day mental problems, including depression, stress and anxiety, can be traced in part to society's increasing alienation from nature. The solution? Get outside and enjoy it.
While traditional psychotherapists focus their treatments on the patient's interior - whether through pharmaceuticals like Prozac, mindfulness practices like meditation, or old-fashioned couch-bound therapy by the hour - practitioners of the burgeoning field of eco-therapy believe that patient care must include time spent in the great outdoors. "It's psychotherapy - as if nature really mattered," says Linda Buzzell-Saltzman, a psychologist and the founder of the International Association for Ecotherapy, which currently lists slightly more than 100 official members.
Eco-therapists point out that human beings have evolved in synchrony with nature for millions of years and that we are hard-wired to interact with our environment - with the air, water, plants, other animals. But in the past two centuries, beginning with the Industrial Revolution, people have been steadily removed from the natural world, our lives regulated not by the sun or moon but instead by the factory clock. Recently it's gotten worse, with the rise of the Internet and other technologies, like iPhones and BlackBerrys, that dominate our lives, pushing us even further from any appreciation of our natural surroundings.
"We began to get the impression that we were somehow above and separate from nature," says Craig Chalquist, an instructor at John F. Kennedy University in San Francisco and co-editor with Buzzell-Saltzman of the new book Ecotherapy: Healing with Nature in Mind.
Today, more than half of the world's population lives in cities, and many people barely ever get a glimpse of green. At the same time, human beings appear to be doing their best to destroy what remains of the earth by contributing to climate change - a problem that in itself causes some people deep anxiety. But what the average person feels as stress or depression, eco-therapists suggest, is a longing for our natural home. "People were embedded in nature once," says Buzzell-Saltzman. "We've lost that, and we're paying the price."
Getting it back doesn't have to be difficult, according to eco-therapists, most of whom, unsurprisingly, practice in California. Patients' treatment typically begins with starting a nature journal, in which they record how much time they spend outside. The results can often be shocking, says Buzzell-Saltzman. "Some patients find they spend less than 15 to 30 minutes a day outside, other than walking to and from their cars," she says. Eco-therapists counsel patients to slow down and reconnect with nature by hiking, gardening or simply taking walks outdoors. Therapy sessions may also take place outdoors - in a park, for example - rather than inside yet another office. "We can use the natural world to be part of the healing process," says Chalquist. "We have to acknowledge that we're part of this, not the master of it."
If such prescriptions sound a little simplistic, consider this: A 2007 study by researchers at the University of Essex in England found that a daily dose of walking outside could be as effective as taking antidepressant drugs for treating mild to moderate depression. Of course, it's no secret that regular exercise is a powerful mood enhancer - although researchers noted that a similar regimen of walking in a crowded shopping mall did not have the same impact - and the boost in vitamin D production in people who spent more time outside in the sun surely helped as well.
It may be that eco-therapy is less a practical psychological treatment than a timely philosophy that connects common feelings of isolation and stress with the fact that the world in which we live is slowly becoming something it shouldn't be. And with worsening climate change and a relentless drumbeat of bad news about our endangered environment, it seems our eco-anxiety may be far from being cured. "Ultimately, what we need to do is change human behavior," says Buzzell-Saltzman - a commonsense recommendation for humans as well as the environment.
------------
"Divorce Hurts Health Even After Remarriage"
Jeanna Bryner, Senior Writer, LiveScience.com - Monday, July 27, 2009
Divorce can wreak havoc on a person's health, even after remarriage, a new study finds.
Scientists have known that marriage can boost a man's health and augment a women's purse. The new study shows that divorce or losing a spouse to death can exact an immediate and long-lasting toll on those mental and physical gains.
"That period during the time that this event is taking place is extremely stressful," said study researcher Linda Waite, a sociologist and director of the Center on Aging at the National Opinion Research Center at the University of Chicago. "People ignore their health; they're stressed, which is itself a health risk; they're less likely to go to the doctor; they're less likely to exercise; they're sleeping poorly."
It turns out, once you have tarnished your health, it's hard to snap back, even if you tie the knot again. "Remarriage helps. It puts you back on a healthy trajectory," Waite told LiveScience. "But it puts you back on a healthy trajectory from a lower point, because you didn't take care of yourself for a year."
Finding that divorce and spousal death had similar impacts on a person's health suggests divorce operates like a traumatic event in one's life, according to Waite.
Mark Hayward of the University of Texas at Austin, who was not invovled in the study, agreed.
"The acuteness of stress surrounding a divorce could operate a lot like a trauma as opposed to years and years of low-grade stress," said Hayward, who is also the director of the university's Population Research Center.
The new study "suggests much of health can be altered by these major turning points in one's life, like divorce, from which one doesn't recover," Hayward said.
Divorce prognosis
Waite and Mary Elizabeth Hughes of the Johns Hopkins Bloomberg School of Public Health in Maryland analyzed data collected from nearly 9,000 adults ages 51 to 61 who took part in the nationally representative Health and Retirement Study.
Overall, about 20 percent of the participants were remarried, meaning they had previously been divorced or widowed, the researchers will report in the September issue of the Journal of Health and Social Behavior. And nearly 22 percent had previously been married but hadn't remarried. Less than 4 percent were never married.
Results showed that those who had been divorced or widowed suffered from 20 percent more chronic health conditions, such as heart disease, diabetes or cancer, compared with individuals who were currently married.
Other findings included:
People who never married reported 12 percent more mobility limitations, such as trouble walking or climbing stairs, than married individuals.
People who never married were 13 percent more likely to show signs of depression than their married counterparts.
Individuals who remarried reported an average of 12 percent more chronic conditions and 19 percent more physical limitations compared with the continuously married. No difference in depression was found between these two groups.
"Some health situations, like depression, seem to respond both quickly and strongly to changes in current conditions," Waite said. "In contrast, conditions such as diabetes and heart disease develop slowly over a substantial period and show the impact of past experiences, which is why health is undermined by divorce or widowhood, even when a person remarries."
What's a couple to do?
The results don't mean spouses should stick together even when the going gets really tough. But during a divorce or after the death of a spouse, people need to make sure to focus on their health, Waite said.
Hayward notes, however, that the results give averages and that some divorces may do a body good.
"If you have a high-conflict, abusive marriage, divorce can be a relief," he said during a telephone interview. "I would never recommend that people in high-conflict, abusive marriages stay in them."
Rather, support during divorce might be key to better health outcomes.
"I'm just suggesting that if there is any room for policy it is to make [divorce] less adversarial and provide more support for those going through the divorce process," Hayward said.
------------
The Boston Globe, Op-Ed, CLAUDIA MEININGER GOLD
"A dangerous label for children"
By Claudia Meininger Gold, August 16, 2009
AS A PEDIATRICIAN who has listened to countless stories from distraught parents, I have no doubt that there are children who, even from infancy, are chronically unhappy. In documenting her struggle with depression in a recent New York Times Magazine article, Daphne Merkin wrote, “It is an affliction that often starts young and goes unheeded - younger than would seem possible, as if exiting the womb I was enveloped in a gray and itchy wool blanket instead of a soft, pastel-colored bunting.’’ My concern, however, with the study in the August issue of Archives of General Psychiatry describing preschool depression is that by saddling these young children with a major psychiatric diagnosis, our thinking will stop. Under the pressure of the powerful pharmaceutical industry, a direct line from diagnosis to drug will be the path of least resistance.
My sense is that these children process the world differently. One mother described carrying her screaming son for hours until she realized that he didn’t want to be held. Another mother said her daughter was “not cuddly’’ and difficult to feed. As they become toddlers, the issues change. I hear about what I call “sock bump anxiety,’’ where many changes of socks are required to find the one with the right seam in the toes. “Fun’’ family outings to a county fair can end in disaster as kids become overwhelmed by all of the sights and sounds. Intense tantrums and meltdowns are frequent.
When I talk with parents of these young children, I often discover that Mom, or Cousin John, or some other relative was just like this as a child, and now has a diagnosis of depression or bipolar disorder. They fear their child will have the same fate. Certainly I cannot claim to know what the future holds for these children.
However, I do have ideas about how to help these families in the present, ideas that are informed by contemporary research at the interface of developmental psychology, neuroscience, and behavioral genetics. This research shows that a child’s mind grows and develops when the people who are most important to the child are able to think about the child’s experience without becoming overwhelmed or shutting down. A parent’s capacity to “hold a child in mind’’ can help that child learn to manage difficult emotions and may actually change the way his brain handles stress.
To help parents with this task, which is more difficult than is generally acknowledged, I first validate their experience. One mother was beaten down by the constant comparisons to her sister’s angelic, easygoing child. “You are not a bad parent,’’ I tell them. “Life is really more challenging for you and your child.’’ If one parent suffers from depression, the strain of such a child can be particularly intense, and that parent will need help for him- or herself.
The normal stress that a child places on a marriage is significantly magnified. One mother of a 6-month-old felt a transformation in her relationship with her daughter simply because her husband came to the visit with me. He finally appreciated what she was experiencing at home while he went to work. With his support she had more energy to be fully present with her child.
All of the burden need not be on the parents. As these children get older, certain types of activities can be particularly helpful. These include martial arts, music, swimming, and horseback riding. I guide parents in finding what is right for their child. One boy at the age of 6 discovered a love for the stage. I joked with his parents that he might grow up to be a great actor, if they could just survive his childhood!
It is quite possible that if I were to list these children’s symptoms, or administer a standardized assessment tool, as was done in the recent study, they would meet diagnostic criteria for “major depressive disorder.’’ But such an approach is oversimplified and misses the nuances and complexities of human relationships. I would offer the same help with or without the label. In my opinion, labeling these young children serves only one purpose: to provide a new market for the pharmaceutical industry.
-
Claudia Meininger Gold, MD, is a pediatrician in Great Barrington.
-
------------
-

-
Molly Boxer, left, holds a candle last night at a vigil for the National Alliance for the Mentally Ill (NAMI) of Berkshire County at Berkshire Community College. The local NAMI chapter is celebrating its 25th anniversary this week. (Caroline Bonnivier Snyder / Berkshire Eagle Staff)
-
"NAMI reaches out to police"
By Dick Lindsay, Berkshire Eagle Staff, Thursday, October 8, 2009
PITTSFIELD -- Local law enforcement will soon be better prepared to deal with the mentally ill in the community.
The National Alliance for the Mentally Ill -- or NAMI -- of Berkshire County is initially training 48 police officers from four different police departments to be part of a crisis intervention team within their city or town. Pittsfield, Adams, North Adams and Egremont are signing up for the inaugural 40-hour training sessions, which will be held in January and again in March at Berkshire Community College.
NAMI officials, which began formulating the training program 10 months ago, expect many more local police departments will enroll their officers in future classes.
"Basically, police want more training because 30 percent of the calls they respond to involve someone with a mental illness," said Molly Boxer, president of the NAMI board of directors.
Training coordinator James Beauregard cited how the crisis intervention model, which began in 1988 in Memphis, Tenn., has a "proven track record" of success 21 years later.
"It's currently in hundreds of cities in 35 states," noted Beauregard.
He added that the training will eventually be offered to state police, the Berkshire County Sheriff's Office, college campus security and emergency medical services personnel.
NAMI's announcement that its newest initiative is going forward comes as the local chapter celebrates its 25th anniversary this week.
The mental health organization held its annual candlelight vigil at BCC last night and will host a gala dinner dance fundraiser on Saturday night, with Gov. Deval L. Patrick the guest speaker.
Boxer said funds raised at the event, which is sold out, will help defray the $40,000 start-up cost for the police training.
NAMI also facilitates support groups, monthly educational meetings and is an overall advocate for the mentally ill and their families.
"We help them navigate the mental health system," said Executive Director Bonnie Brace. "It's very tricky to do."
Carol -- not her real name -- discovered three years ago how important NAMI is to the Berkshires. She said a teenage family member was not getting the help he needed, until she called the NAMI office.
"Bonnie was the first person I talked to," Carol told an Eagle reporter after the vigil. "She gave me such a confidence right away."
Carol added, NAMI were not only advocates for the now-16-year-old boy, but also helped her and other family members "understand mental illness, how to cope with mental illness and accept it."
"The hardest thing is accepting someone has mental illness," noted Mary Rowland, a child and adolescent specialist for NAMI.
Rowland has been working Carol's case and found marked improvement in the 16-year-old who regularly attends a local high school.
"We're unsure when he'll get his diploma," added Rowland. "The ultimate goal is to have a happy, healthy adult who's productive in the community."
-
To reach Dick Lindsay: rlindsay@berkshireeagle.com, or (413) 496-6233.
-
www.topix.net/forum/source/berkshire-eagle/TMU83ACP42FHJL0RV
-
------------
-

-
Dr. Hisham Hafez, executive director and chief medical officer at the Greater Nashua Mental Health Center, is seen in a clinical exam room. Hafez received news of a $2 million grant to establish partnerships with primary care physicians.
-
"Mental health center gets money to integrate primary care"
The Nashua Telegraph, November 2, 2009
These days it might almost seem the doctors and therapists are almost rolling in money at the Greater Nashua Mental Health Center at Community Council. They aren't, but this month the center received two grants to expand homeless prevention and mental health programs and a third, multimillion dollar grant to become one of 13 sites in the country trying to integrate physical health care into a behavioral health setting.
The largest grant, $2 million over four years from the Substance Abuse and Mental Health Services Administration, will allow Community Council to staff a fully equipped exam room at its 7 Prospect St. facility and establish partnerships with primary care clinics and health centers in the area.
“This is really exciting for us,” Dr. Hisham Hafez, Community Council's executive director and chief medical officer, said. “This is something we're very proud of and I think Nashua should be proud.”
The program is an experiment of sorts, according to Mara Huberlie, who works in Community Council's development office. While the integration of behavioral and physical health care is seen as the future, most past efforts have tried to move behavioral health into a primary care setting.
“Integrated care is the new thing. It's the future,” Huberlie said. “It has to be. It doesn't make sense to have these different silos.”
The $500,000 a year will pay to hire a nurse practitioner to see people who are suffering from severe mental health problems and are already receiving treatment at Community Council. A primary care physician will oversee the entire program while a nurse supervisor will work to coordinate patient care and direct them to other therapies Community Council and the program's community partners have for other issues, such as substance abuse, Huberlie said. The idea is for data from all 13 sites to be aggregated and studied to determine if integrating physical health care into a behavioral health setting works more effectively than the reverse. At the same time, best practices will be established in case it is more effective, Huberlie said.
Sufferers of mental illness are at risk for a number of health conditions including obesity, substance abuse, diabetes and smoking, which reduces their life expectancy by about 30 years, Hafez said. Their mental illness also often makes those conditions worse in sufferers, Hafez said, because they are less likely to see a primary care physician or be effective participants in their own health care.
“This is a public health problem we need to address,” Hafez said. “We need to monitor their mental health and physical health together because ultimately that's what recovery is.”
The program is scheduled to start in February, Huberlie said, and until then Community Council will be trying to iron out partnership agreements with health care providers around the state, including Southern New Hampshire Medical Center, Nashua Area Health Center and the Lamprey Health Care in Newmarket.
The grant is part of almost $26 million given to fund similar programs in Kentucky, Colorado, California, Ohio, Connecticut, New Jersey, Arizona, Illinois, New York and Oklahoma, according to the Substance Abuse and Mental Health Services Administration.
“Physical health problems among people with serious mental illnesses impact their quality of life and contribute to disproportionate premature deaths,” said Eric Broderick, acting administrator of the Substance Abuse and Mental Health Services Administration. “These community programs will help address disparities in treatment by providing more people in need with better access to screening and care management, including wellness programs, encouraging more physical activity, better nutrition, smoking cessation and help with medications.”
The other grants Community Council received are smaller and will expand existing programs.
A 24-month, $200,000 Bureau of Justice Assistance grant was awarded to the center, through Hillsborough County, to expand the Community Connections Mental Health Court Project into Manchester District Court. Community Council will work with the Mental Health Center of Greater Manchester on the project, according to Susan Stearns, Community Council's director of development.
The court is a diversion program that allows people who suffer from mental illness to avoid jail time if their illness directly led to their infractions. In return, defendants are required to stay out of further trouble and stick to a counseling and rehabilitation program. The hope is that the opportunity to get better, as opposed to going to jail or prison, will break the cycle of petty crime, jail, release and more petty crime. It is a cycle that costs taxpayers untold thousands of dollars a year.
The grant will pay for a court liaison, who will work with police, prosecutors, defense attorneys, judges, defendants and mental health experts to help design counseling regimens that, if followed, allow nonviolent offenders to avoid jail time.
The grant will also pay for that liaison in Nashua, Scott Brennan, to work for the court full-time. He will be able to help establish the program in Manchester and work with defendants suffering from mental illness in district courts in Milford and Manchester, Stearns said.
The hope is that data generated during the grant will show the savings the program brings to the Hillsborough County House of Corrections and that county leaders will continue funding the program, countywide, once the grant expires, Stearns said.
The third grant, for $200,000 over three years, will expand Community Council's Place to Live program, that subsidizes rent and utility payments for mental illness sufferers who are on a waiting list for Section 8 housing, Stearns said. The stimulus money is being distributed through HUD's Homelessness Prevention Program, she said.
Stearns said mental illness is one of many risk factors for homelessness, and once people become homeless, the majority of them become involved in the criminal justice system within a year.
Community Council will use the money to pay out the subsidies to 20 people for up to 18 months, Stearns said.
-
Joseph G. Cote can be reached at 594-6415 or jcote@nasuatelegraph.com.
-
------------
"When mentally ill are prone to violence"
The Boston Globe, Letters, February 5, 2010
RE “KERRIGANS faced dilemma with adult son’’ by Peter Schworm and Milton Valencia (Metro, Jan. 27): It is true that many families are forced to deal alone with mental illness and substance abuse. However, Marylou Sudders, president of the Massachusetts Society for the Prevention of Cruelty to Children, is wrong to suggest that individuals with mental illness are no more violent than the general population. People with severe psychiatric disorders who are being effectively treated are no more likely than the general population to be violent. The issue, however, arises when people are not getting the medication they need.
Multiple studies have demonstrated that individuals with severe psychiatric disorders who are being inadequately treated, or not treated at all, are more likely to be violent than the general population. In fact, being severely mentally ill and not taking medication is one of three major clinical predictors, along with past history of violence and substance abuse, of violent behavior. Often, the victims of violence are the mentally ill individuals themselves. The second most likely victims are family members.
Massachusetts has one of the most outdated civil commitment laws in the country. The citizens of Massachusetts deserve the changes proposed by state Representative Kay Khan in a bill that would bring much-needed reform to the mental health treatment laws in the Commonwealth.
Kristina Ragosta
Legislative and policy counsel
Treatment Advocacy Center
Arlington, Va.
-
www.boston.com/bostonglobe/editorial_opinion/letters/articles/2010/02/05/when_mentally_ill_are_prone_to_violence/?comments=all#readerComm
-
------------
"Grief Could Join List of Disorders"
By BENEDICT CAREY, N.Y. Times, January 24, 2012
When does a broken heart become a diagnosis?
In a bitter skirmish over the definition of depression, a new report contends that a proposed change to the diagnosis would characterize grieving as a disorder and greatly increase the number of people treated for it.
The criteria for depression are being reviewed by the American Psychiatric Association, which is finishing work on the fifth edition of its Diagnostic and Statistical Manual of Mental Disorders, or D.S.M., the first since 1994. The manual is the standard reference for the field, shaping treatment and insurance decisions, and its revisions will affect the lives of millions of people for years to come.
In coming months, as the manual is finalized, outside experts will intensify scrutiny of its finer points, many of which are deeply contentious in the field. A controversy erupted last week over the proposed tightening of the definition of autism, possibly sharply reducing the number of people who receive the diagnosis. Psychiatrists say current efforts to revise the manual are shaping up as the most contentious ever.
The new report, by psychiatric researchers from Columbia and New York Universities, argues that the current definition of depression — which excludes bereavement, the usual grieving after the loss of a loved one — is far more accurate. If the “bereavement exclusion” is eliminated, they say, “there is the potential for considerable false-positive diagnosis and unnecessary treatment of grief-stricken persons.” Drugs for depression can have side effects, including low sex drive and sleeping problems.
But experts who support the new definition say sometimes grieving people need help. “Depression can and does occur in the wake of bereavement, it can be severe and debilitating, and calling it by any other name is doing a disservice to people who may require more careful attention,” said Dr. Sidney Zisook, a psychiatrist at the University of California, San Diego.
In blogs, letters, and editorials, experts and advocates have been busy dissecting the implications of this and scores of other proposed revisions, now available online, including new diagnoses that include “binge eating disorder,” “premenstrual dysphoric disorder” and “attenuated psychosis syndrome.” The clashes typically revolve around subtle distinctions that are often not readily apparent to those unfamiliar with the revision process. If a person does not meet precise criteria, then the diagnosis does not apply and treatment is not covered, so the stakes are high.
“The world has changed” since the last revision, in 1993, said Dr. James H. Scully Jr., chief executive of the psychiatric association. “We’ve got electronic media around the clock, and we’ve made drafts of the proposed changes public online, for one thing. So anybody and everybody can comment on them, at any time, without any editors.”
Many doctors and therapists approve of efforts to eliminate vague, catch-all diagnostic labels like “eating disorder-not otherwise specified” and “pervasive development disorder-not otherwise specified,” which is related to autism. But a swarm of critics, including two psychiatrists who oversaw revisions of earlier editions, has descended on many other proposals.
“What I worry about most is that the revisions will medicalize normality and that millions of people will get psychiatric labels unnecessarily,” said Dr. Allen Frances, who was chairman of the task force that revised the last edition.
Dr. Frances, now an emeritus professor at Duke University, has been criticizing the current process relentlessly in blog posts and e-mails. Dr. Robert L. Spitzer, who oversaw revision of the third manual in 1980, has also voiced concerns, as have the American Counseling Association, the British Psychological Society and a division of the American Psychological Association. Some of the concerns have to do with important technical matters, like the statistical reliability of diagnostic questionnaires. Others are focused on proposed changes to the most familiar diagnoses.
Under the current criteria, a depression diagnosis requires that a person have five of nine symptoms — which include sleeping problems, a feeling of worthlessness and a loss of concentration — for two weeks or more. The criteria make an explicit exception for normal grieving, which can look like depression.
But the proposed diagnosis of depression has no such exclusion, and in the new study, Jerome C. Wakefield of New York University and Dr. Michael First of Columbia concluded that the evidence was not strong enough to support the change. “An estimated 8 to 10 million people lose a loved one every year, and something like a third to a half of them suffer depressive symptoms for up to month afterward,” said Dr. Wakefield, author of “The Loss of Sadness.” “This would pathologize them for behavior previously thought to be normal.”
But Dr. David J. Kupfer, a professor of psychiatry at the University of Pittsburgh School of Medicine and the chairman of the task force making revisions, disagreed, saying, “If someone is suffering from severe depression symptoms one or two months after a loss or a death, and I can’t make a diagnosis of depression — well, that is not being clinically proactive. That person may then not get the treatment they need.”
Another point of growing contention is a proposed new diagnosis, “attenuated psychosis syndrome,” which would be given to people who experience delusional thinking and hallucinations and sometimes say things that do not make sense. Psychosis is the signature symptom of schizophrenia, typically a lifelong, disabling mental disorder. Psychiatrists have long hoped for a way to catch it early, before it turns into full-blown schizophrenia.
But critics say these symptoms are poor predictors of the disorder. In studies, 70 percent to 80 percent of young people who report these strange experiences do not ever qualify for a full-blown schizophrenia diagnosis, yet the label increases the risk of being “treated” with powerful anti-psychosis drugs.
“There’s already overuse of these drugs in children and adolescents, and having this vague diagnosis, regardless of its intent, will only increase misuse in this vulnerable population,” said Dr. Peter J. Weiden, director of the psychosis treatment program at the University of Illinois at Chicago.
Some outside experts say the same is true of other proposed additions, like premenstrual dysphoric disorder (lethargy and other depressive symptoms in the week before menses, among other things) and binge-eating disorder (out-of-control bingeing, complete with self-loathing). Getting the diagnosis increases the likelihood of being treated for what is normal behavior, or close enough.
Task force members argue differently: if a person is in distress and seeking help, then treatment ought to be offered — and covered by insurance.
For now, these revisions are still in play; the completed manuscript is due to the printer in December. In the longer term, the politicking is likely to have a corrosive effect on the process, some experts said. Recent findings in genetics show that nature does not respect psychiatric categories — many different disorders seem linked to some of the same genetic glitches.
Already a federal agency, the National Institute of Mental Health, has set up its own independent effort to classify mental disorders, called Research Domain Criteria, which will not be based on existing categories.
In time, said Dr. Steven E. Hyman, a resident scholar at the Broad Institute of M.I.T. and Harvard, this kind of approach should ground the field more in nature and less in expert opinion. Until then, there is and will be the diagnostic manual.
------------
"Holmes to have limited mental health options: Specialists say psychiatric care poor in prisons"
By Dan Elliott and Nicholas Riccardi, Associated Press, July 17, 2015
DENVER — Whether James Holmes gets life without parole or a death sentence for the Colorado theater shooting, he will spend years behind bars, joining about 6,000 inmates in Colorado and hundreds of thousands of others nationwide who suffer from mental illness.
Specialists say prisons are ill-equipped to treat the growing number of inmates with mental illnesses, including the majority who are not convicted of crimes as violent as Holmes, who was diagnosed with a form of schizophrenia.
A jury on Thursday convicted the 27-year-old former neuroscience graduate student of murder and other charges for his 2012 assault at a midnight screening of a Batman movie that killed 12 and wounded dozens of others.
The same jurors will decide his sentence in the penalty phase of the trial, which starts Wednesday and will take about a month. Even if they decide Holmes should be executed, as prosecutors want, he would spend years in prison as his mandatory appeals play out in court.
Holmes pleaded not guilty by reason of insanity, but jurors rejected the claim after two state-appointed psychiatrists testified he could distinguish right from wrong, Colorado’s test for sanity.
But the two state psychiatrists and two defense psychiatrists agreed he suffers from mental illness.
If jurors had found Holmes was insane, he would have been committed indefinitely to a state mental hospital. Instead, he could end up at the San Carlos Correctional Facility, Colorado’s 250-bed prison for inmates with mental illness, where specialists agree his treatment will be at a far lower standard than if he were hospitalized.
‘‘In most hospitals, you don’t have staff whipping out Tasers and pepper spray and using it on their patients,’’ said Jamie Fellner of Human Rights Watch, who has studied mental health treatment in prisons and recently wrote a report detailing instances of mentally ill prisoners being beaten or so violently restrained that they die. ‘‘This kind of treatment isn’t just restricted to someone who’s committed a horrific crime.’’
Last year, Colorado’s Department of Correction approved a $3 million settlement to resolve a lawsuit from a family of an inmate with a form of schizophrenia who died after being restrained in the San Carlos prison. Staffers were videotaped joking as Christopher Lopez suffered seizures and died. The agency said it fired three people.
A spokeswoman for the Department of Corrections said no one was available to comment Friday on the prison system’s mental health care.
People with mental illness sometimes wind up in jail because law officers don’t know what else to do with them, said Scott Glaser, executive director of the Colorado chapter of the National Alliance on Mental Illness.
And once in the criminal justice system, they find it hard to get out.
‘‘They cannot usually get effective treatment,’’ Glaser said. ‘‘It increases recidivism. If someone is dealing with a mental illness that affects their decision-making. It’s very easy for them to end up in the system again.’’
Nationwide, a 2006 federal study estimated that 56 percent of all prisoners in state custody suffered from mental illness and 15 percent suffered from some sort of psychotic disorder. Mental health advocates say their treatment is almost uniformly substandard for a variety of reasons.
Mentally ill people do not fare well in the crowded, loud environment of prisons, the study concluded. They are more likely to have trouble following rules, which makes them more likely to be punished and end up in solitary confinement.
The isolation of a solitary cell can vastly aggravate their mental illness. They are also more likely to be victims of sexual abuse, the study said.
Colorado lawmakers banned solitary confinement for inmates with serious mental illness after a prisoner who had been held in solitary for much of his eight-year term was suspected of killing the state prisons chief, Tom Clements, in 2013.
‘‘Prison is a pretty horrific place to be, especially if you have a mental illness,’’ said Laura Usher of the National Alliance on Mental Illness’ national office.
The incarceration of mentally ill inmates in jails and prisons has been a persistent national problem since the widespread closure of mental hospitals in the 1970s.
A local community care system to handle the newly released mentally ill never materialized, and now they often end up behind bars. There the Constitution entitles them to basic medical treatment, said Dr. Renee Binder, president of the American Psychiatric Association, but it’s often hard to meet that standard.
The APA and other groups are pushing for more programs to keep the mentally ill out of prison initially — be it those special courts or local treatment.
‘‘When someone ends up in jail and prison and has a serious mental illness, it’s really a problem with the system,’’ Binder said. ‘‘The question needs to be asked: ‘Could we have prevented this?’’’
------------
“Ending stigma is key to mental health fight”
The Berkshire Eagle, Letters, October 5, 2015
To the editor:
Mental Illness Awareness Week is Oct. 4 through Oct. 10. We at the National Alliance on Mental Illness of Massachusetts (NAMI Mass) want people to be aware of the fact that mental health conditions affect one in four adults. We want people to know that these disorders are treatable, but according to the Substance Abuse and Mental Health Services Administration (SAMHSA) in Massachusetts only 52.8 percent of our adult population received treatment.
A key reason why people don't seek treatment is stigma. With a recent initiative, NAMI Mass is trying to combat this problem through the workplace.
Although it is well-documented, most people are unaware that mental health issues are the leading cause of disability in the workplace. We learned through a statewide survey that only 27 percent of employees in Massachusetts are willing to talk about their mental illness at work. CEOs Against Stigma, NAMI's campaign, is trying to affect change by meeting with CEOs of companies throughout Massachusetts and promoting empathy and a supportive environment for employees no matter what illness they have.
We hope more CEOs will sign on so we can win the battle against stigma and more individuals can experience hope and recovery.
Laurie Martinelli, Boston
The writer is executive director, NAMI Massachusetts
------------
Letter: “Together we can address tragedy of suicide”
The Berkshire Eagle, March 23, 2019
To the editor:
It's with a heavy heart that I write this letter today. It feels as if our community has been struck a mighty blow with the sheer number of recent losses to suicide, as well as the family murder/suicide. Our hearts are with the families and friends, while the trauma extends to many hundreds of impacted lives from these losses. It's a time when we need to lean into each other and ask ourselves.... What more can we do as a caring and compassionate community?
We can comfort those who are bereaved, by listening quietly without judgment or oversimplified statements. We can suggest resources found at www.berkshirecoalition.org such as an outreach visit or the peer support group for suicide loss. The group meets monthly on the 1st Thursday from 5:30-7 p m at Berkshire Children & Families, in the Family Resource Center, at 480 West Street in Pittsfield.
We can acknowledge that suicide is a complex tragedy when multiple stressors converge and are heightened by a period of escalated mood and behaviors. We can do our best to keep at-risk individuals safe and offer to bring them to get help. Call the Lifeline at 800-273-TALK(8255) if you're worried about someone and want to learn more. There's even a crisis counselor available 24/7 by texting 741-741. These resources are for anyone, whether you are feeling suicidal or concerned about someone else.
What else can a concerned citizen do? We can come to terms with the fact that suicide is a public health issue that needs to be addressed with community conversation as well as advocating for improved mental health services. Several Berkshire organizations have collaborated to offer a full day Suicide Prevention Conference on Friday, April 5 — "Fostering Resiliency and Enhancing Connection." While the training does offer continuing education hours for licensed professionals, it's also designed for all community members to recognize and facilitate protective factors. The registration deadline has been extended and scholarships are available. Go to www.berkshirecoalition.org to register.
Our vision is for everyone to find an alternative to suicide and self-harm, to find relief from unbearable psychological pain, and for our community to meet their needs. By working together we can find solutions to the gaps in urgent mental health care, find more effective ways to help individuals build resilience to stress, and better care for each other, including our selves.
Peggy Morse, Pittsfield
The writer is a suicide prevention advocate, Berkshire Coalition for Suicide Prevention (BCSP).
------------
“Coping with isolation, stress”
By Jenn Smith, The Berkshire Eagle, March 28, 2020
Fever, coughing and fatigue aren't the only adverse symptoms of the new coronavirus pandemic.
As jobs are lost, people are isolated and kids are stuck at home from school, we become susceptible to increased levels in hormones like adrenaline and cortisol, elevated heart rate and blood pressure, increased muscle tension and faster or more shallow breathing — all physiological symptoms of being in a state of crisis or stress.
When Berkshire Pathways, a clubhouse program of Viability Inc., which supports people with mental health diagnoses, had to shutter its door to help prevent COVID-19 spread, program Director David Brien said his staff was prepared to function under a "new normal," but some members were thrown for a loop.
"They crave the social support they get in coming here," he said. "A lot of them broke down in tears because they were not going to have that physical place of support that they've come to for years. One member still comes by a couple of times a day just to wave hello through the window."
Now, Berkshire Pathways staff are working to fill the gaps by delivering daily lunches, taking phone calls from and checking in on members remotely.
Even people who don't have an existing mental health disorder are prone to feeling vulnerable and could struggle to cope with all the disruption to their daily routine and lifestyle.
"We're all being asked to rapidly adapt to something totally new. For some people, this will give them a sense of a loss of control. It's harder for some than it is on others," said Jane Tillman, a board certified clinical psychologist and psychoanalyst for Austen Riggs Center in Stockbridge.
Becca Phelps-Smith is a licensed clinical social worker and the director of emergency and acute care services for The Brien Center. She oversees the center's Emergency Services Program and Crisis Team, and says her staff has been experiencing an uptick in the volume of calls, including new callers, to the crisis line.
"It's been hard because we don't have all the answers ... and we don't have a lot of good information about what happens next," Phelps-Smith said.
"Our own brains get out of control when we start to think what might happen," said Melody Fisher, a Berkshire Community College associate professor of psychology and former community health clinician.
Fear and unconscious stress stimuli could cause us to lash out, curse more, eat more junk food or lose sleep. Unless we find an intervention, the effects of chronic stress could lead to longer term health problems like lasting anxiety, depression, addiction, obesity, clogged arteries and could even damage the cells of the immune system.
During this time of prolonged crisis, local mental and behavioral health experts say they fear a subsequent uptick in domestic violence, including child abuse, as well as an increase in the number of people experiencing thoughts of suicide.
"We need to slow that process down and learn how, during times of tension, to get some space," Tillman said.
"Just using the word 'pause,' is a good place to start," Fisher said, noting how emotions can manifest in and overwhelm the body.
"Just breathing in through the nose — 1, 2, 3, 4, 5 — and slowly out through the mouth tells your brain I'm safe enough to breathe slowly. It really does engage the parasympathetic response," she said, referring to the part of the nervous system that slows the heart rate and relaxes the gut.
Building structure and daily routine, even if it's just eating or taking a break at the same time of day can be helpful, Fisher said.
"Art and spirituality can be in a place of uncertainty and fear. That's what they're there for, as a way of feeling connected and comforted," she said.
The experts all agree that limiting news consumption, developing a nutritious diet, maintaining regular sleep and exercise habits, and staying connected with loved ones through technology can all help improve mental and physical health and reduce the risk of harming oneself or others. But developing these habits also requires discipline.
For some people, this means not overindulging in food and drink or not over-committing to helping others. For some it will mean learning to walk away when angry, or learning to listen versus arguing, or learning to set boundaries and time limits.
"We hear a lot about self-care, right? But self-care is not always about bubble baths and chocolate. Sometimes it's about doing something hard, right now," Fisher said. "Relative ease in the world isn't a given."
But choosing wisely how to use our time and energy can help create better outcomes.
"Structure really helps people across the board," Phelps-Smith said.
Jenn Smith can be reached at jsmith@berkshireeagle.com, at @JennSmith_Ink on Twitter and 413-496-6239.
Support resources available 24/7
In an emergency, call 911.
Berkshire Crisis Team: 413-499-0412
Suicide Prevention Lifeline: 1-800-273-8255 (TALK)
Samaritans Statewide: 617-247-0220
Text a crisis counselor: 741-741
Trevor Help Line for LGBTQ support: 1-866-488-7386
Veterans Crisis Line: 1-800-273-8255 and press "1," or text 838-255
Substance Abuse and Mental Health Services Administration's (SAMHSA's) Disaster Distress Helpline: 1-800-985-5990 or text "TalkWithUs" to 66746. (TTY 1-800-846-8517)
Elizabeth Freeman Center: 866-401-2425
Additional regional support NAMI Berkshire County: For support, call 413-443-1666 or email namibc@namibc.org, or visit https://namibc.org/resources for an expanded directory of resources and services.
Berkshire Pathways: 413-464-7949
Berkshire Coalition for Suicide Prevention: https://berkshirecoalition.org
Berkshire District Attorney's Office is also posting a number of resources, from health to legal service informatoin, via Facebook: https://www.facebook.com/BerkshireDA/
In their words ...
Here's what some Berkshire County residents said in response to a Facebook post about what people are doing to cope during this crisis:
"I'm taking advantage of online prayer and meditation services from the Shrine of Divine Mercy in Stockbridge."
— Jim Massery
"Journaling, writing, deep cleaning, meditating, stretching, taking walks outside. Solo yoga, long baths, cooking, lots of cooking."
— Isabella DeLuca
"I've been working on perfecting a cold foam to put on my cold brew coffee. It is a silly thing to do, but I look forward to getting up and making my morning coffee. It's a nice treat and a nice way to start my day."
— Veronica Bosley
"While working remotely and in between virtual meetings, I'm getting a lot of reading done and will probably cruise by my goal of reading 50 books this year!"
— Kelan O'Brien
"Dance parties on Zoom with our grandchildren who live in New York and California but we are now connected for movement therapy every day for 45 minutes taking turns picking out songs ( which "Alexa" plays for us)...we can't stop laughing."
— Christine Singer
------------
Letter: Marijuana use worsens our mental health crisis
The NH Union Leader, May 19, 2021
To the Editor:
Everyone, including the governor, seems surprised that New Hampshire has a mental health crisis. But the crisis will become even worse, because no one is addressing one of the major causes — marijuana use among our youth, as young as 8 years old.
Even without legalization, marijuana use by our youth is 26% higher than the national average. In Carroll County, it is 66% higher.
Why is marijuana causing mental health problems? Because today’s marijuana is 10 times stronger in THC than in the 1970s and 1980s. Marijuana today actually rewires the brain in youth and young adults under 25 creating psychosis (loss of reality), schizophrenia, violence, depression, suicide, and more.
Therefore, you have a mental health crisis as well as joblessness, homelessness, bullying, physical abuse to children, and aggravated assaults. Read the studies.
Couple that with lung cancer, heart attacks and strokes, and damaged immune systems, and marijuana becomes a death sentence, not a recreational drug. Look at the states that legalized marijuana years ago: Hawaii, California, Washington, Oregon, Colorado. Mental health problems and homelessness abound. One step is a statewide Drug Prevention campaign focused on marijuana, required under NH Law (Chapter 12J), but ignored by the NH Commission on Alcohol and Other Drugs and the NH Prevention Task Force. They spend millions every year! You haven’t seen their Drug Prevention ads because there are none. In 2017, Governor Chris Sununu said prevention “Stinks.” Four years later, prevention still stinks, governor.
Bob Batson, Wolfeboro
------------
"For South County health care workers, a lesson in substance use disorder stigma"
By Francesca Paris, The Berkshire Eagle, June 11, 2021
Gary Pratt has felt the weight of addiction stigma — even inside the walls of a hospital.
A snide comment from a doctor. A side eye from a phlebotomy technician. A judgmental remark from the front desk.
Pratt, now in long-term recovery, knows how damaging that stigma can hurt people just trying to get back on their feet. Any of these seemingly minor interactions could discourage someone with substance use disorder from seeking help, he says, and slam shut that tiny, crucial window when that person was able to commit to recovery.
That’s why Berkshire Community College and Rural Recovery Resources have teamed up to train South County health care and social service professionals to deal more effectively and empathetically with addiction, approaching each patient as someone suffering from a chronic brain disease.
“It’s 2021, and a lot of people are still stuck in the moral model of treatment,” said Pratt, project manager for Rural Recovery Resources. “‘This is something you did to yourself, you’re not really deserving of treatment.’”
The five-week, 10-hour curriculum at BCC aims to reduce stigma by training everyone from social workers to hospital receptionists in everything from the latest science of addiction to motivational interviewing. The course, “Foundations of Opioid Addiction and Recovery,” is taught by Kari Dupuis and Pam Coley McCann, human services faculty at BCC.
“I feel probably all of us, in some way, shape or form, have some stigma around mental health and recovery,” Dupuis said. “Education is a critical component.”
The training, which began in May, includes lessons on compassion fatigue, the impact of substance use disorder on friends and family, evidence-based treatment, harm reduction and more. Guest speakers have included local experts, and people with experiences of addiction and recovery.
“There’s a lot of harbored bias toward patients in recovery,” said Elena Nuciforo, BCC’s director of workforce development for health care. “If you’re on your first day of recovery and you see someone who rolls their eyes, even nonverbal signals, you might walk away. You might think, ‘People just don’t have any faith in me.’”
Nuciforo thinks that, sometimes, stigma arises when a health care worker knows someone in their personal life who has struggled with substance use disorder, and she hopes just reframing the facts about the disease can help participants overcome negative stereotypes.
“Let’s say you have a son or nephew who died of overdose,” Nuciforo said. “You think ‘junkies’ drug him into this, you’re really angry ... a lot of negative feelings. But, there’s also a lot of times a lack of understanding about addiction. Not just in the lay population, but among health care providers.”
The course will run five more times, including once again this fall, and Pratt hopes to reach as many health care and social service workers as possible.
These trainings are part of a broader effort by Rural Recovery Resources and the group’s partners to confront the ongoing opioid crisis. Opioid-related overdoses killed 56 people in Berkshire County last year, a record number, and the epidemic has touched the lives of many more.
The Human Resources and Services Administration has awarded a $1 million grant to the South Berkshire Opioid Consortium — made up of Berkshire Community College, The Brien Center, Fairview Hospital and the Railroad Street Youth Project. That money is going to education, prevention and improved screening, among other projects, all intended to build resources and community in the southern Berkshires.
“A lot of substance use disorder screening hasn’t been happening,” Pratt said. “We want it to be as innocuous as domestic violence screening.”
The money also is going toward a bricks-and-mortar peer-support recovery center in Great Barrington, which will serve as a one-stop shop to refer people to resources and a space to host meetings.
Rural Recovery Resources already has rented a space and started weekly “all recovery” meetings, Pratt said. He hopes to open its doors formally in the coming months, after renovations to the building.
South County health care professionals looking for more information about the Foundations of Opioid Addiction and Recovery training sessions can contact Nuciforo at enuciforo@berkshirecc.edu or Gary Pratt at gary@rsyp.org.
------------
May 23, 2022
Hello Editor(s) of the NH Union Leader,
People with mental health symptoms that cause mental illness are no more violent than people without mental health symptoms. There is no causal correlation between mental illness and violence in society, nor has there ever been. People with mental health symptoms that cause mental illness should receive evidenced based mental health care to treat their mental health symptoms. Mental health patients often work to live a functional and healthy life in society, and their mental health recovery is often a lifelong journey.
As for people who are experiencing homelessness, there should be a continuum of care group of government agencies, not-for-profit organizations, and religious institutions who will help homeless people and families find safe shelters. People and families in need should learn to build a community support network whereby they give and receive support to help each other.
The deinstitutionalizing of mental health patients was replaced by the jail and prison system of mass incarceration. The new mental health institutions are where people with mental illness are behind bars. Wall Street, corporations and career politicians all profit off of incarcerating people with mental illness. The police, court system, and jails and prisons unfairly bear the burden of caring for people with mental illness. Mental health care has become punitive instead of being about mental health care.
The insurance and pharmaceutical industry see mental health patients as numbers on their financial spreadsheets instead of vulnerable people and families who need housing, mental health care and community support. State governments spend over 50 percent of their state budgets on health care, while the federal government spends over 34 percent of their federal budget on health care, but the only big winners are insurance company and pharmaceutical executives who give millions of dollars to the corrupt career politicians to grow their profit margins.
Every other industrialized country has universal healthcare except for the U.S.A. No other country has the gun violence epidemic on the scale that the U.S.A. has. If one wants to blame someone or something for "The Mental Health Epidemic", look no further than big government and the insurance and pharmaceutical industries.
Jonathan A. Melle
-----
"Mental illness: A new epidemic"
NH Union Leader, Editorial, May 22, 2022
Writing in his Wall Street Journal column last week, Daniel Henninger warned that the next big epidemic after COVID-19 will involve mental health.
Noting the accused mass murderer in Buffalo, Henninger said the focus should be on the suspect’s mental illness issues, rather than his “white power” ranting.
The warehousing of the mentally ill a generation ago was replaced, not with help, but with a “deinstitutionalization” whose promise of community care was hollow. As a result, the “mentally homeless are piling up on the streets of San Francisco, Los Angeles, New York, Austin and on and on.”
He could add Manchester, Nashua, Concord, etc. to the list.
We must do better with a mental illness epidemic than the government did with COVID.
That means more voices at the table, not just the public health establishment.
------------













































































































































.png)