http://projects.washingtonpost.com/staff/articles/alec+macgillis/
-
----------
Analysis
"About Those Clinton Primary Voters"
By Alec MacGillis
Democrats have been wringing their hands since yesterday about one seemingly daunting figure in new polls showing a tightening of the presidential race.
Obama, according to the polls, is still having trouble locking down the votes of Hillary Clinton's primary-season supporters. An NBC/Wall Street Journal poll found that only about half of self-identifying Clinton supporters backed Obama, while a fifth are backing John McCain and fully a quarter remain undecided.
Some are interpreting this as evidence that Obama has a lingering problem with the Democratic base, and even speculating that he consequently might shock the world and pick Clinton as his running mate.
Lost in this analysis, though, is a crucial fact: many of Clinton's primary-season supporters are not necessarily loyal Democratic presidential election voters.
Indeed, many of the states and counties where Clinton racked up her biggest numbers in the primaries are places where voters remain Democrats in name only (think Kentucky). Such voters may have turned out to participate in an exciting 2008 Democratic primary, but they have not voted for Democrats in recent presidential elections, and can hardly be considered part of the Democratic base.
Take Beaver County in western Pennsylvania, where the New York Times today found strong resistance to Obama among Clinton supporters and Obama lost to Clinton by a whopping 40 percentage points during the primary. If Obama does not win all those voters back, he will hardly be the first: Democrats outnumber Republicans in the county 68,000 to 35,000, yet [John] Kerry won the county by only 2.7 percentage points. And despite losing so many of the county's Democrats to George W. Bush, Kerry nonetheless carried Pennsylvania.
To be sure, Clinton would have done better with Democrats in places like Beaver County than Obama will, and Obama needs to run as close to even in such locales as he can. But they were never going to be his path to victory in the Keystone State, where he is instead counting on Philadelphia and its suburbs -- a region that has been growing while western Pennsylvania shrinks -- and big margins among African Americans, younger voters and independents.
As well, Obama is not even competing in the general election in some of the states where Clinton won big totals against Obama in the primaries. Clinton beat Obama by 250,000 votes in Kentucky, and by 150,000 votes in West Virginia. Both are states where Democrats still outnumber Republicans by huge margins -- and yet Bush both won handily in 2004.
----------
-

-
Al Gore's speech touched on a favorite topic, climate change, saying Barack Obama is prepared to address "a planetary emergency." (Photo Credit: By Preston Keres -- The Washington Post). 8/29/2008.
-
"Gore Delivers a Boost -- To Obama and a Pet Cause"
By Alec MacGillis, Washington Post Staff Writer
Friday, August 29, 2008; A18
DENVER, Aug. 28 -- In the past three decades, Al Gore has come to the Democratic National Convention in many roles -- as an ambitious young senator, a vice presidential candidate, a vice president and a presidential nominee. On the last night of the 2008 convention, he came as a Nobel Prize-winning proselytizer against the perils of climate change, linking Barack Obama's candidacy to his own cause of the past decade.
With an allusion to his prize-winning documentary on climate change, he argued in a speech at Invesco Field at Mile High on Thursday that Obama, unlike Sen. John McCain, is prepared to address the issue that Gore called a "planetary emergency."
"His experience," Gore said, "has taught him something that career politicians often overlook: that inconvenient truths must be acknowledged if we are to have wise governance."
Gore said the race between McCain and Obama is as close as it is "because the forces of the status quo are desperately afraid of the change" Obama represents.
At a convention that witnessed the remarkable drama of both Hillary and Bill Clinton forcefully endorsing Obama and, in essence, passing the party's baton to someone who was not on the stage until four years ago, the former vice president's role fits less neatly into the narrative.
Gore was Clinton's vice president, but furious over the Monica S. Lewinsky scandal, he made less use of the president on the campaign trail in 2000 than many had expected, further cooling their relationship. His loss to George W. Bush despite a popular-vote plurality represented a totemic and devastating "what might have been" moment for Democrats. Thursday night, Gore returned to it, listing all the ways in which, he argued, the country would have fared better under his leadership.
But since the loss, he has reinvented himself as a world spokesman warning about climate change. He shared the 2007 Nobel Peace Prize with the United Nations' Intergovernmental Panel on Climate Change and won an Oscar for his documentary, "An Inconvenient Truth."
Gore remained neutral in this year's Democratic nomination battle, and as the contest between Obama and Hillary Rodham Clinton dragged on, his name was often invoked as someone who could broker a resolution between them. He endorsed Obama after he had captured the nomination, appearing with him in June.
"He's said many times that [the primary battle] was historic and exciting . . . and that in the end result it would be good for the Democratic Party, that it would energize a lot of people and bring a lot of new people out," said Michael Feldman, a political consultant with the Glover Park Group in the District and a longtime Gore adviser. "He expected all along that this would resolve itself elegantly and organically -- and it did."
Carol M. Browner, head of the Environmental Protection Agency in the Clinton administration and a close Gore associate, described his frame of mind in similar terms. "I think he's very happy with where we are. We have a nominee, a spectacular nominee, and he's going to do everything he can to see him elected," she said.
Obama campaign manager David Plouffe said the campaign wanted Gore in as prominent a spot as possible.
"We think Gore can deliver a compelling message on both the economy and foreign policy as relates to energy," Plouffe said. "He's a messenger. There are a lot of elected officials that voters don't readily accept information from, and he's one that they do. They think that he's got credibility. He has some credibility because a lot of voters believe that if he were elected, the last eight years would have been different."
Plouffe refused to say whether Gore had been considered as Obama's running mate. Some Democrats speculate that Obama, if he wins, could appoint Gore to a new position, of climate change czar.
But Feldman said Gore appears to think he is having the most impact in his current role outside government, which includes giving speeches, working on several green energy investment ventures, and leading a new initiative to have the United States producing all its electricity from renewable and noncarbon sources within 10 years. That goal has been derided by many Republicans and is far more ambitious even than the aggressive target laid out by Obama.
"What he has said is that he is not interested in serving in a future administration but that he hasn't ruled out public office, and that if he ran for office again it would probably be for president. He hasn't said, 'Under no circumstance will I serve the country again,' " Feldman said. "He has found a very unique role and platform as a kind of public-private citizen, able to harness resources creatively to make a huge impact on the climate crisis."
Browner agreed. "He obviously is a very influential person with [Obama], and he'll continue to be that, but [Obama] will make the decision as to who joins his administration," she said. "What Al is passionate about is the issue of climate change . . . and my guess is the most effective place for him is using his talent for speaking out about the issue, raising concern and inspiring people to take action."
----------
"Stimulus Aid Being Doled Out, Slowly: Meeting Guidelines Is Taking Time"
By Alec MacGillis, Washington Post Staff Writer, Friday, April 10, 2009; A01
Building repairs are underway on public housing in Imboden, Ark., and Cumberland, Ill., states across the country are receiving money to weatherize the homes of low-income residents, and the Silver Star Construction Co. is about to start work on two road-resurfacing projects in south-central Oklahoma with a total cost of $12 million.
"We were thrilled to get some work," said Steve Shawn, president of the company. "Some of the work had started slowing down from the economy. The new work came in just around the right time."
Slowly but surely, the $787 billion American Recovery and Reinvestment Act -- better known as the economic stimulus package -- is beginning to percolate nationwide, six weeks after President Obama signed the legislation.
Some of the money is arriving quickly, and in big chunks. The country's 1,100 community health clinics have received $337 million to help them handle the surge of newly unemployed and uninsured people needing care. An additional $155 million went to a more select group of 126 of the clinics, including $1.3 million for the Loudoun Community Health Center, which, after opening in 2007, has been seeing an increase in demand even though it is in an affluent area of Northern Virginia.
In most cases, though, the money is working its way into the system far more gradually as officials strive to meet not only existing guidelines for programs receiving aid but also reporting requirements that have been added to make sure that stimulus funding is spent as intended and to account for the jobs it creates.
As a result, White House officials say the bulk of the money will start hitting the streets later this year and early next, with the goal of spending 70 percent of it by the summer of 2010. As of Tuesday, $54 billion from the package had been "obligated," meaning that states, cities or other recipients could begin drawing from it, and $11.7 billion of that had been disbursed.
The $11.7 billion is not the full extent of the money in circulation, however. The Transportation Department, for instance, has distributed very little, but states have started on some highway work in anticipation of money they are slated to receive. Also, those figures do not include the boost that employees started seeing in their paychecks at the start of this month from the package's Making Work Pay tax credit.
"We've been pretty pleased" by the pace of spending so far, said Robert Nabors, deputy director of the Office of Management and Budget. "I know people are anxious to get started, and the money has started to flow out the door. But we're spending a lot of time planning . . . and trying to make sure we've put processes and a structure in place to be sure we're spending on the right priorities."
The balance between taking enough time to plan for the money and not unduly delaying actual spending goes to the central tension in the legislation, which sought to jump-start the economy and also to make progress on Obama's long-term agenda. The package included $201 billion in tax cuts, $87 billion in Medicaid funding, $79 billion in education funding, $28 billion for highways, $21 billion for food stamps, $17 billion to computerize health records, $11 billion to modernize the electric grid, $17 billion for rail and public transit, and $20 billion to increase the energy efficiency of homes and public buildings.
With more than 100 funding streams contained in the package, many officials find themselves having to file applications for several programs at a time, helping explain why much of the money is still months away from being spent.
Take, for instance, what Oregon's Housing and Community Services Department needs to do to secure its $82 million. It has already applied for $38 million to weatherize low-income residents' homes, and just received the first 10 percent of that, but still needs approval from the state legislature to spend it. It is awaiting guidelines for applying for $27 million in tax credits for affordable housing development. It just received the guidelines for applying for $8 million to help prevent homelessness, and expects that it will not spend that money before July.
And Oregon will not apply until July for "neighborhood stabilization" funding that will be
distributed on a competitive basis for states to renovate or demolish abandoned homes. In fact, it is still getting ready to spend $19.6 million that it received for a similar purpose from a housing recovery bill President George W. Bush signed in late July.
It is a lot of hoops to jump through, but officials say it is worth it. "This is a huge investment for us," said Rick Crager, Oregon's deputy housing director. The process "is not an issue for us. It's important that we're accountable."
Peter Grace, a special assistant to the secretary of Housing and Urban Development, said it takes time to develop rules for new programs. "We want to get this money out, we are committed to doing that, but we want to do it in a thoughtful way," he said.
Likewise, the Energy Department is releasing only a fraction of the $6 billion that states and cities are receiving to increase energy efficiency, and is requiring that they submit detailed plans for using the money before they get the bulk of it.
There is little immediate spending going on even in departments that are using money on their own, instead of parceling it out to states. The Interior Department is still deciding how to spend its $3 billion, as its Bureau and Land Management and its National Park Service scour the hundreds of possible renovation projects for those that are far enough along in the permit process to merit receiving money. It hopes to have a list ready by May 1.
"What you've got is an unprecedented operational process combined with an unprecedented -- and appropriate -- level of review, and that's taking time," said Chris Henderson, the department's stimulus expert.
Among those getting money out relatively fast is the Transportation Department, which was able to rely on its existing formulas to divvy up $48 billion among states. Lana Hurdle, a deputy assistant transportation secretary, said the department has so far obligated $6.3 billion, with more to come soon -- states must obligate half their money within 120 days or risk having to return some of it. Leading the pack was Oklahoma, which obligated half its $460 million in 28 days.
Still, much of the actual road work will take time to ramp up. Missouri was fast out of the gate, saying that a bridge rebuilding contract awarded in February was the country's first stimulus project. But some of the 37 contracts it has awarded will not break ground anytime soon. The overhaul of the Interstate 70 and 435 interchange in Kansas City still needs environmental and public approvals, and probably will wait until early next year for the gap between the football and baseball seasons, because the interchange is near the sports stadium.
The delays extend even to one of the smallest stimulus projects in Missouri, $167,000 for sidewalks on the main road through Cleveland, a town of 650 on the Kansas line south of Kansas City. The town may not have the paperwork in place for work to begin until late this year, said its volunteer mayor, Patricia Masterson.
Still, the project has boosted spirits.
"We were very surprised and very pleased. It will connect our city a little bit more. Right now, we mostly walk around in our own neighborhood rather than getting out," she said. "It helps to show that everyone is going to get something. It shows, yes, this will get down to the grass roots and it is not all going to stay in the big cities."
----------
"In Retooled Health-Care System, Who Will Say No?: Questions About Cost And Limits Linger"
By Alec MacGillis, Washington Post Staff Writer, Wednesday, July 8, 2009
The question came from a Colorado neurologist. "Mr. President," he said at a recent forum, "what can you do to convince the American public that there actually are limits to what we can pay for with our American health-care system? And if there are going to be limits, who . . . is going to enforce the rules for a system like that?"
President Obama called it the "right question" -- then failed to answer it. This was not surprising: The query is emerging as the ultimate challenge in reining in health-care costs that now consume $2.5 trillion per year, or 16 percent of the economy. How will tough decisions be made about what to spend money on? In a country where "rationing" is a dirty word, who will say no?
The question permeates all levels of medicine: the use of tests that many argue are unnecessary (U.S. doctors order five times as many MRIs as doctors do in Germany); how early to intervene with common conditions such as heart disease and prostate cancer; how aggressively to treat patients nearing their life's end.
Although Obama and his advisers have held up providers' spending patterns as the crux of the crisis, proposals in Washington go only so far in addressing the thorniest questions about who gets what care. Instead, cost-saving measures are focused on introducing a public insurance option to compete with private insurers, or on general cuts in Medicare and Medicaid payments to hospitals.
The bills being written would put new emphasis on evaluating treatments according to their "comparative effectiveness," or weighing the risks and benefits of different types of treatment for the same illness, but the bills stop short of incorporating cost-benefit analyses into the findings or of requiring that providers abide by conclusions.
Lawmakers are also considering ways to reform Medicare payments to emphasize the overall quality of care over the quantity of treatments. But lawmakers are not going as far as Massachusetts did; it is considering shifting entirely from a fee-for-service model to one where salaried physicians would be paid an overall annual price for covering a given person or family.
Such a shift would probably be a shock to the system of many Americans, who have grown used to having any and all health-care options, regardless of cost, available to them.
"The questions of who gets what, these difficult choices . . . really are not posed in the current health reform legislation," said Drew E. Altman, president of the Kaiser Family Foundation. "The challenge," he said, "is us, the American people: We want the latest and the best, and we want it now."
The Democrats' caution has not kept Republicans from accusing them of embracing rationing. They raise the specter of the British agency, which goes by the acronym NICE, that decides whether that country's nationalized health-care system will pay for items such as costly cancer drugs that extend lives a few months on average.
"You're going to be saying to people, 'We're not going to care for you, because we've decided it's too expensive to care for you,' " said Robert E. Moffit of the right-leaning Heritage Foundation.
Others retort that the United States already has rationing: The uninsured and under-insured do not get the care they need. "We're already doing it," said Stanford University epidemiologist Randall Stafford. "We're just doing it in such way that it doesn't service societal interests."
But reformers are clearly spooked by the notion that they could be accused of denying, for example, hip surgery to an 80-year-old. In recent months, a federal panel has held hearings on how to spend $1.1 billion in economic stimulus money allocated for comparative effectiveness research. At each hearing, representatives of providers, industry and patient groups praised the research -- but then demanded that cost not factor into the eventual findings.
Scott Wallace, a Bush administration official who is now the Batten Fellow at University of Virginia's Darden School of Business, said factoring cost into treatment decisions would create the same backlash that HMOs encountered in the 1990s. "A mother of five with cancer wins against any rationing scheme ever created," he said.
Many physicians and health care-experts argue, though, that it is precisely by marshaling better research data, partly with the help of electronic health records, that a case can be built for limiting certain treatments. If doctors were to demonstrate to heart disease patients how few advantages coronary artery bypass graft surgery has over less expensive treatments, for example, many patients probably would not elect to undergo the surgery.
At Kaiser Permanente, the California-based health network that relies heavily on such research, Permanente Foundation Executive Director Jack Cochran said fears of treatment denials were exaggerated. Doctors, he said, need to be more realistic about not raising vain hopes about expensive, last-ditch treatments: "Comparative effectiveness is a hot-button issue because everyone sees their pieces of pie coming under scrutiny. But all of our pieces should be under scrutiny."
All signs in Washington suggest that cost considerations will be kept at arm's length as health-care legislation moves forward. Carolyn M. Clancy, director of the Agency for Healthcare Research and Quality, said the emphasis will be on clinical outcomes alone.
The draft legislation in the Senate Health and Education Committee, meanwhile, stresses that any research findings "shall not be construed as mandates for payments in coverage and treatment."
A senior administration official who requested anonymity to speak candidly acknowledged that while research might point to obviously wasteful practices, the reform would for the time being not get at the "harder question" of what to do "if new technology does work better and reduces risks but costs a lot more, and how to evaluate that."
The other half of the "saying no" challenge, reformers agree, is giving providers the right incentives and structures to deliver high-quality care as affordably as possible. The goal is to spread the "accountable care" models featured by the Mayo Clinic and others, where a network of providers works closely together to coordinate a patient's care, increasing the odds of keeping them healthy and decreasing unnecessary procedures.
Massachusetts, which has achieved near-universal health coverage but is struggling with high costs, is considering major changes in this direction. A legislative commission is about to release a report recommending that the state goad providers into joining networks that would receive payments for each enrollee, rather than for each procedure delivered.
Proponents say it would differ from the "capitation" approach -- fixed payments for each member -- used by the HMOs in the past because there would be more focus on performance and long-term value than on simply keeping costs down.
Skeptics say such a system would force the state's many solo practitioners or small groups of physicians into big networks and would renew complaints from the HMO era about limiting patients' choice. In Massachusetts, for instance, most parents with a sick child would demand access to Children's Hospital; and most cancer patients would want to go to the Dana-Farber Cancer Institute, no matter what network those were in.
The plans being considered in Washington do not go nearly as far in seeking to change providers' spending habits. They contemplate changing some Medicare payments from fee for service to a "bundling" system in which providers would be paid for an entire episode of care, giving them an incentive to reduce repeat hospital admissions. Another idea is to empower the Medicare advisory panel whose recommendations now tend to be ignored by Congress, or to create a separate, Federal Reserve-like entity to make tough decisions about federal health-care spending.
John C. Goodman, president of the conservative-leaning National Center for Policy Analysis, questions this approach, citing new research by his group that shows that areas with high Medicare spending do not correlate with high medical spending overall, suggesting that fixing excesses in Medicare will not necessarily translate to the broader system.
Henry J. Aaron of the Brookings Institution, who co-wrote a 2006 book called "Can We Say No?" said that real cost reform would mean giving all physicians incentives to leave behind the fee-for-service model for accountable care networks. The transition will take a long time, he said, and at first, people could still sign up for fee-for-service plans. But they would see their neighbors getting good care at a much lower price and hopefully switch over themselves.
"We're just not going to be able to all have everything . . . regardless of cost," Aaron said.
----------
"The Unwitting Birthplace of the 'Death Panel' Myth"
By Alec MacGillis, Washington Post Staff Writer, Friday, September 4, 2009
LA CROSSE, Wisconsin -- This city often shows up on "best places to live" lists, but residents say it is also a good place to die -- which is how it landed in the center of a controversy that almost derailed health-care reform this summer.
The town's biggest hospital, Gundersen Lutheran, has long been a pioneer in ensuring that the care provided to patients in their final months complies with their wishes. More recently, it has taken the lead in seeking to have Medicare compensate physicians for advising patients on end-of-life planning.
The hospital got its wish this spring when House Democrats inserted that provision into their health-care reform bill -- only to see former Alaska governor Sarah Palin seize on it as she warned about "death panels" that would deny care to the elderly and the disabled. Despite widespread debunking, those warnings have led lawmakers to say they will drop the provision.
"It's really distressing," hospital official Bud Hammes said. "These things need to be addressed."
President Obama's health-care initiative was nearly consumed by the furor over that provision, and Republicans continue to argue that the legislation would ration care for the elderly. The debate has underscored how fraught the discussion is on end-of-life care in a country where an optimistic ethos places great faith in technology and often precludes frank contemplations of mortality. That tendency has a price tag: A quarter of Medicare costs -- totaling $100 billion a year -- are incurred in the final year of patients' lives, and 40 percent of that in the last month.
But the controversy has had most resonance where it arguably took root, in this town of 52,000 where nearly everyone of a certain age has an advance-care directive.
La Crosse became a pioneer in addressing end-of-life questions in the mid-1980s, after Hammes, a native of the city who has a doctorate in philosophy from Notre Dame, arrived at Gundersen as the director of medical humanities, charged with educating resident physicians about ethics. He noticed a "troubling pattern," he said, in which family members struggled to make medical decisions, such as whether to continue dialysis after a stroke.
"We'd turn to the family and say, 'We need your input. If your mother or father could speak now, what would they tell you?' And the family would say, 'If we only knew,' " said Hammes, 59. "I could see the distress. They were going to have to live with themselves, with the worry about making a mistake. This was unacceptable."
The hospital began urging families to plan while people are healthy. For those who want help writing a directive, a physician will discuss the powers and limits of medicine and explain to family members what it means if they agree to serve as the "health-care agent." They will also help people define the conditions under which they would no longer want treatment. Hammes said people often define this as "when I've reached a point where I don't know who I am or who I'm with, and don't have any hope of recovery."
The directives are power-of-attorney forms that protect physicians and family members against liability, and the hospital makes clear to its doctors that they are expected to follow them. Today, more than 90 percent of people in town have directives when they die, double the national average.
The reliance on directives has an impact on the type of care people receive: Gundersen patients spend 13.5 days on average in the hospital in their final two years of life, at an average cost of $18,000. That is in contrast with big-city hospitals such as the University of California at Los Angeles medical centers (31 days and $59,000), the University of Miami Hospital (39 days, $64,000) and New York University's Langone Medical Center (54 days, $66,000).
Those disparities are not explained just by the hospital's end-of-life philosophy. Under Medicare formulas, Gundersen and other Upper Midwest hospitals receive lower reimbursements. The high-spending hospitals argue that they are also dealing with a more diverse and costly patient base.
Gundersen and other Upper Midwest providers are also less costly in general, partly because they follow a model of integrated care where doctors work closely together to minimize waste. At Gundersen, doctors receive a salary instead of being paid for each procedure they perform.
But locals say the city uses less health care in large part because of how people view the end of life. Some of this may be rooted in the down-to-earth sensibility of their German and Scandinavian forebears. (Hammes said his late mother, who had dementia, was a "pragmatic German" who thought that paying to keep herself alive was a "waste of her money.")
Mostly, though, locals say it is because Gundersen and the town's other hospital, Franciscan Skemp, have urged planning. "People here have their feet planted in the ground," said Barbara Frank, a retired teacher. "They're no-nonsense sorts of people, without a lot of illusion. That was the fertile soil upon which it was planted. But there's no question it was helped by the two medical centers taking the lead and saying, 'This is a good thing for you to do.' "
She and her husband, Donald, a retired train engineer, signed a directive 10 years ago, when they were in their 60s. "You increasingly realize that they're not going to make an exception in your case. We all die, and we want to do so with the most dignity and most control," she said. "It seemed a no-brainer. And it spares our children from making those decisions."
Over time, the practice caught on. "People talk to people who talk to people. They say, 'Do you have one?' 'Yeah,' or 'I have to get that done,' " said Ann Kotnour, a nurse whose 89-year-old mother is receiving care at home for her advanced Parkinson's after signing a directive in 2001 saying she did not want aggressive measures taken.
Financial planner Jeff Lokken's parents had met with their children and doctors in the mid-1990s to draw up directives, a step that was helpful a few years later, when he and his siblings needed to decide whether to keep their 77-year-old father on a ventilator after heart surgery. The living will also helped when his mother's health failed when she was 82. "There needs to be a conversation. In our case we had good conversations," he said.
But Gundersen staff members say those conversations take a lot of time -- a good hour, plus follow-up talks to alter directives as medical situations evolve. And Medicare does not reimburse doctors for the time spent on such discussions.
Backed up by a few other hospitals, Gundersen set out to change the federal rules to reward end-of-life planning. A Gundersen administrator testified on Capitol Hill last fall, and, with the help of a lobbyist, reached out to lawmakers such as Sen. Herb Kohl (D-Wis.), Sen. John D. Rockefeller IV (D-W.Va.) and Rep. Ron Kind (D-Wis.).
After sporadic bipartisan attempts in recent years to add consultation payments to Medicare, Rep. Earl Blumenauer (D-Ore.) submitted legislation this spring, with several Republican co-sponsors, that included a provision to reimburse doctors for consultations. A few months later, House Democrats tucked similar language into their health-care reform bill -- a legislative triumph for the small hospital in La Crosse.
Then the uproar began, capped by Palin's "death panel" remark. Gundersen officials and town residents were aghast. "It's totally absurd," Frank said. "It's just the opposite -- it's giving you a choice of how you want to be treated."
Gundersen officials were particularly upset when Sen. Charles E. Grassley (R-Iowa), whom they had considered an ally, said that the government should not "pull the plug on Grandma" and that the provision would be dropped. They were also dismayed when the provision was criticized by former House speaker Newt Gingrich (R-Ga.), who had been open about how much he appreciated the end-of-life care his father-in-law received at Gundersen.
Rep. Paul D. Ryan (R-Wis.) admires Gunderson generally but said it erred in pushing for Medicare to cover consultations. "It's right and proper for Gundersen to innovate in these directions, but it's a wholly different thing for the federal government" to endorse end-of-life planning, he said.
Gundersen officials are still fighting to keep consultation payments in the bill, with support from Sen. Mark Warner (D-Va.), who has become a leading advocate for such planning. But this week, word came that the White House is willing to drop the provision. The hospital officials are even less hopeful about more ambitious terms they sought to add -- changing Medicare payments for end-of-life care so that they are based not on the procedures a patient receives in the final months but on whether care complied with the person's wishes.
No matter what, they will keep trying to get payment for consultations into future legislation. "The [directive] itself doesn't really matter very much -- it's the clearly expressed belief and shared understanding that it represents," Hammes said. "The family members have to believe that what they do is not only legally right, but personally right. If Mom said, 'Don't do this or do do this,' it's much easier for them to say, 'I'm doing a loving thing,' and it's a decision you can live with."
The discussions do not promote less aggressive care, he said: "We're not trying to talk them into anything. We're trying to understand their values and goals, and tell them what medical science can and can't do." But many people do settle on less care. "In our community," he said, "people don't want to die hooked up to machines."
----------
-

-
Speaker Nancy Pelosi is joined by Majority Leader Steny Hoyer and Rep. George Miller after the House health-care bill passed Saturday. (Photo Credit: Alex Brandon / Associated Press Photo).
-
"Abortion an obstacle to health-care bill: Some Democrats vow to block final passage if amendment stays"
By Alec MacGillis, Washington Post Staff Writer, Monday, November 9, 2009
President Obama and Senate Democrats sought on Sunday to generate momentum from the House's passage of health-care legislation, even as a new hurdle emerged: profound dismay among abortion-rights supporters over antiabortion provisions inserted into the House bill.
The House passed its version of health-care legislation Saturday night by a vote of 220 to 215 after the approval of an amendment that would sharply restrict the availability of coverage for abortions, which many insurance plans now offer. The amendment goes beyond longstanding prohibitions against public funding for abortions, limiting abortion coverage even for women paying for it without government subsidies.
The abortion issue had been rumbling within the House Democratic caucus for weeks, but Saturday's votes revealed the depths of the fault lines. The amendment passed with the support of 64 Democrats, roughly a quarter of the party caucus.
But abortion-rights supporters are vowing to strip the amendment out, as the focus turns to the Senate and the conference committee that would resolve differences between the two bills.
Although House liberals voted for the bill with the amendment to keep the process moving forward, Rep. Diana DeGette (D-Colo.) said she has collected more than 40 signatures from House Democrats vowing to oppose any final bill that includes the amendment -- enough to block passage.
"There's going to be a firestorm here," DeGette said. "Women are going to realize that a Democratic-controlled House has passed legislation that would prohibit women paying for abortions with their own funds. . . . We're not going to let this into law."
Senate Majority Leader Harry M. Reid (D-Nev.) is waiting for cost estimates of provisions of the bill he is cobbling together, and hopes to bring it to the Senate floor before Thanksgiving. The battle over abortion has been more muted in the Senate, but Jim Manley, Reid's spokesman, predicted that would change.
"The debate in the House highlighted some of these issues that we're going to have to face here in the Senate, and on this issue in particular, it's something [Reid] is going to have to talk with his caucus about," Manley said.
Obama left the abortion issue unmentioned Sunday when he appeared in the Rose Garden to give brief remarks congratulating the House on its "courageous" passage of the bill. "Now it falls on the United States Senate to take the baton and bring this effort to the finish line on behalf of the American people," he said. "And I'm absolutely confident that they will."
Other issues remain unresolved. The House bill's primary new revenue source to pay for the bill is an income tax surcharge on families earning more than $1 million; the Senate bill will probably rely on a proposed new excise tax on costly insurance plans. The House and Senate also differ on a government-run insurance plan to be offered on the new marketplace where small businesses and people without employer-provided coverage -- about 30 million in all -- would buy coverage.
The Senate bill would limit this "public option" by allowing states to opt out of it, but even in that form its prospects are unclear. Sen. Joseph I. Lieberman (I-Conn.), whose vote Democrats will probably need to break a filibuster, warned again Sunday that he will withhold his support if the bill includes a public option.
The bills also differ in their requirements for employers to provide coverage -- the House's language is tougher -- and in the subsidies for those who cannot afford coverage, which are larger in the House bill. The House version also does not contain language included in the Senate bill that would bar illegal immigrants from receiving subsidies and also from buying coverage on the new marketplace themselves.
On CBS's "Face the Nation," Sen. Lindsey O. Graham (R-S.C.) said the fact that more than 30 conservative Democrats voted against the bill bodes poorly for it in the Senate, where conservative Democrats have more power. "The House bill is dead on arrival in the Senate," he said. "It was a bill written by liberals for liberals."
The abortion debate in the House has centered around how to put the bill in compliance with the ban on taxpayer funding for abortions. Rep. Lois Capps (D-Calif.) proposed that a government-run plan and private plans offered in the new marketplace for people without employer-based coverage could offer abortion coverage, but payments for abortions would come out of premiums, not the government subsidies for those who need help buying coverage.
Antiabortion groups argued that such a segregation of funds would be a mere accounting gimmick. After a compromise foundered, the amendment by Rep. Bart Stupak (D-Mich.) and Joe Pitts (R-Pa.) emerged as the leading alternative, with the strong backing of the U.S. Conference of Catholic Bishops. The amendment would prohibit abortion coverage in the government-run plan and any private plan on the new marketplace that accepts people who are using government subsidies to buy coverage.
Under that language, abortion coverage would be unavailable not only to working-class women buying coverage with government subsidies, but probably also to women buying coverage on the new marketplace without federal assistance. The amendment suggests that women could buy separate "riders" covering abortions, but abortion-rights supporters say it is offensive to require a separate purchase for coverage of a medical procedure that is for most women unexpected.
Charmaine Yoest, president of Americans United for Life Action, hailed the wide margin for the amendment. "I said all along that the inclusion of abortion as health care was going to be a political conflagration," she said.
But Nancy Keenan, president of NARAL-Pro Choice America, said that although the vote was "extremely disappointing and outrageous," the "fight isn't over." DeGette said she remains hopeful that the amendment will be dropped as more Democrats who voted for it -- and their constituents -- realize it goes beyond the status quo of limiting federal funding for abortions. Some of those House Democrats are not against abortion rights, just against federal funding, and she surmised that they may have misunderstood the amendment.
She said her House allies have requested a meeting with Obama, saying they "need him to back us up" after lying low on the issue.
"This would be the greatest restriction on a woman's right to get an abortion with her own money in our lifetime," she said. "The stakes could not be higher."
----------
"Abortion amendment in House bill raises questions"
By Alec MacGillis, The Washington Post (Online), Saturday, November 14, 2009 3:00 PM
After the House passed its health care bill last weekend, debate exploded over an amendment by Rep. Bart Stupak (D-Mich. ) and Rep. Joe Pitts (R-Pa.) that restricts abortion coverage.
Confusion was rampant all week, but on this both sides agree: the debate reflects the conflict between the rule banning federal funding for abortions, and the expansion of the government's role in health care. Universal health care is a Democratic and liberal goal, but as long as the ban stands, increasing government support for those who lack insurance likely means more restricted coverage for abortions.
Richard Doerflinger, spokesman for the U.S. Conference of Catholic Bishops, has been trying to explain this irony to religious conservatives who worry "that when the federal government takes over health care, it'll be pro-death." In fact, he said, "When you expand the reach of federal funds, you expand the reach of federal policies" on abortion.
Here are answers to some questions about the amendment.
1. What is the status quo? Under the 33-year-old federal ban, there is no abortion coverage under Medicaid, the federal employee health benefits plan or the TRICARE plan for military families. Seventeen states use their own funds to provide abortion coverage for Medicaid recipients. A study co-authored by the Guttmacher Institute, which backs abortion rights, found that women on Medicaid were 25 percent more likely to carry an unwanted pregnancy to term if they did not have abortion coverage.
Abortion coverage is widespread among private insurance plans -- at least half of people with private coverage have abortion coverage, according to surveys by Guttmacher and the Kaiser Family Foundation. Guttmacher found that only 13 percent of abortions are billed directly to a private insurer, though many women bill their insurers separately. An abortion at 10 weeks costs $400, though it can be far more costly later on.
2. What does Stupak-Pitts say? Under the House bill, people without employer-provided coverage and small businesses would choose among private insurance plans and a government insurance plan, or "public option," offered on a new marketplace, or "exchange." As initially written, these plans would pay for abortions out of people's premiums, and not with any subsidies that will be extended to families who earn up to $88,000 annually. Abortion rights opponents derided this as an accounting gimmick, and turned to Stupak-Pitts. It decrees that abortion may not be covered in the public option or in any of the exchange's private plans that take the subsidized customers. There is an exception if a woman's life is in danger or in cases of rape or incest.
Private plans could offer abortion coverage to those without subsidies, but that will be a small subset of the 30 million people expected in the exchange. Women could also buy a "rider" for abortion coverage, as is now done in a few states where employer-based plans are not allowed to cover abortion. Abortion rights supporters say relying on such riders is unrealistic and offensive, given that few women expect to have an abortion.
3. What does it mean for women? For women who do not have health insurance, gaining subsidized coverage will mean they will be much better off overall, while still lacking abortion coverage. But there are many women who now have coverage on the individual market that is overpriced and low-quality but does cover abortion. Their subsidized coverage under the legislation will be superior in general, but they will lose their abortion coverage, unless they buy a rider. Abortion opponents note this outcome is no different than when Democrats now push to expand Medicaid in the 33 states without abortion coverage.
The impact is less clear for women buying coverage on the exchange without subsidies. This will include higher-income women and those working for small businesses, who likely will not qualify for subsidies since their employers will be helping pay. For these women, the availability of a plan covering abortion will depend on whether insurers decide to offer a plan that is open to only some people and differs from other plans only in covering abortion -- not the easiest distinction to market.
Such a plan could also upset the balance envisioned for the exchange, with costs shared across plans -- the plan would draw members unlike any other, wealthier and with more more women in child-bearing age.
Some higher-income women may choose to go without abortion coverage, on the assumption that they could pay for it out of pocket. But they could then find themselves facing the high cost of an abortion with complications.
4. Are there broader implications? Abortion-rights advocates worry abortion foes will apply the amendment to other federal funds in the bill, such as tax credits for small businesses or subsidies for companies with early-retiree plans. But the amendment's supporters say this is not their intent. Abortion rights advocates also worry that as insurers introduce plans on the exchange without abortion coverage, they will for convenience's sake drop it from their employer-provided plans. Abortion opponents counter that insurers customize many of their plans today.
Most notably, larger businesses will eventually be able to join the exchange, and more people may come to the exchange on their own if their employers drop coverage outright. As the exchange grows in size, the abortion restrictions will apply to more people -- though the market for plans limited to the non-subsidized customers will also grow.
5. Will the amendment stick? Many Senate Democrats hope to pass language closer to the original House language, paying for abortions out of premium funds. Separating private and public funds in the exchange's plans, abortion rights supporters say, is no less an accounting scheme than the Catholic Church's segregation of federal funds it gets for school costs from its religious operations, a comparison abortion foes reject. Forty House Democrats now say they will reject a final bill with the amendment.
But at least one Senate Democrat, Nebraska's Bill Nelson, wants the amendment. And Democrats are struggling to find language that is less restrictive and yet satisfies the two dozen House Democrats who voted for the bill but want assurance that it truly upholds the federal ban.
President Obama has said he wants the bill to uphold the status quo on federal funding and abortion, but also said that he thought Stupak-Pitts went too far -- leaving him in the same bind as many fellow Democrats.
----------
"Both sides question health bill's abortion compromise"
By Alec MacGillis, Washington Post Staff Writer, Tuesday, December 22, 2009; A08
The abortion language that was added to the Senate's health-care bill to win the vote of Sen. Ben Nelson (D-Neb.) has achieved a rare feat: It is drawing contempt from both sides.
That could be taken as a sign that senators finally found an elusive compromise on a thorny issue. But serious questions are already being raised about how the new language would work in practice and whether it would even be feasible to implement.
"This is why it's being attacked by both sides -- not because it's so moderate but because it's crazy," said Richard Doerflinger, a spokesman for the U.S. Conference of Catholic Bishops.
Sara Rosenbaum, a George Washington University professor of public health and law who criticizes the language as too restrictive, echoes that conclusion: "None of how this is supposed to work is even remotely in the bill, so I don't know what people are thinking about it."
The long-standing ban on federal funding for abortion has complicated congressional Democrats' health-care legislation. Medicaid bars federal funding for abortion, but 17 states and the District allow the procedure for female Medicaid enrollees paid out of their own funds. It is harder to reach middle ground in the bill before Congress, which would provide federal subsidies to millions of people to buy private health insurance plans on a new marketplace, or "exchange." The deal reached by Nelson and other Democrats over the weekend would allow those people to purchase insurance plans with abortion coverage. But they would have to write two separate premium checks -- one to cover the bulk of their plan and the other to cover the sliver for abortion coverage, probably a dollar or so per month.
States could also decree that no plans including abortion coverage be provided on the exchange in their state. As it stands, five states already have some sort of ban on abortion coverage.
By contrast, an amendment that passed the House would prohibit insurers from selling plans with abortion coverage to anyone buying coverage with the help of subsidies -- excluding 85 percent of customers on the exchange. The amendment, sponsored by Reps. Bart Stupak (D-Mich.) and Joe Pitts (R-Pa.), would permit the sale of "riders" for abortion coverage, but abortion rights groups say it is offensive to expect women to buy separate coverage for a procedure that most do not plan on needing.
Neither the House language nor the Senate language would affect women who have employer-provided plans, many of which cover abortion. But it is expected that more people would go into the exchange over time for coverage, broadening the impact of its rules.
An amendment by Nelson that mirrored the Stupak-Pitts language failed in the Senate. Senators supporting the new language say it is preferable to Stupak-Pitts because it would allow all women, subsidized or not, to buy plans with abortion coverage, assuming their state allows it.
"Is this the language we wanted? No. But it stopped Stupak and kept health reform moving forward without rolling back women's health-care options," said Alex Glass, a spokeswoman for Sen. Patty Murray (D-Wash.).
Others outside the Senate, though, say the language could limit abortion coverage as much as Stupak-Pitts. Anyone who selects a plan that includes abortion coverage would have to pay two separate premiums -- even single men or older women, who would not need abortion coverage. Abortion rights supporters suggest that would prompt frustration and, in turn, reduce demand for such plans. Eventually, they argue, insurers may decide not to offer abortion coverage at all.
"The absurdity of requiring these two separate checks doesn't accomplish anything toward the supposed goal of segregating federal funds," said Cecile Richards, president of the Planned Parenthood Federation of America. "It just creates additional hoops for insurance companies . . . and more administrative burdens and obstacles for women to get the coverage they need."
Jake Thompson, a spokesman for Nelson, said the senators crafting the compromise had not consulted with insurers. "As far as what insurers might do, that's hypothetical," he said.
Insurance representatives said it is too soon to say how the language would shape their offerings. But Wellpoint spokeswoman Kristin Binns noted that the insurer already navigates different rules in offering products in 14 states. "We comply with all the regulations, so however they pan out, we'll comply accordingly," she said.
To abortion opponents, the new language is objectionable simply because it would permit federal subsidies for people who buy plans with abortion coverage. They are not reassured by the prospect that insurers may find the language so unwieldy that they would stop offering such coverage.
"This is so murky that it's difficult to predict how it would be implemented," said Douglas Johnson, legislative affairs director for the National Right to Life Committee.
If the Senate bill passes, it will be up to a conference committee to come up with a solution. Stupak, who got 64 Democrats to vote for his amendment, has already declared the Senate language "unacceptable."
----------
"Obama meets with union leaders to discuss health-care reform"
By Alec MacGillis, Washington Post Staff Writer, A03, January 12, 2010
President Obama sought on Monday evening to assuage organized labor's misgivings about the health-care overhaul, even as several key union leaders warned that the bill's final outlines could severely dampen their enthusiasm for the Democratic ticket in this year's elections.
Obama invited 10 labor leaders to the White House to discuss the negotiations aimed at reconciling the Senate and House bills, which are not heading in organized labor's direction in the three areas that it had identified as priorities. The final bill will not include the House's government-run insurance plan, or "public option"; it will probably include the Senate's new tax on high-cost health plans that could affect many union members; and its penalties for employers who do not provide insurance coverage will probably be closer to the more lenient terms in the Senate bill.
Three hours earlier, AFL-CIO President Richard Trumka said in a hard-edged speech at the National Press Club that discontent with the final bill, when combined with a general perception that Obama and Congress have been insufficiently populist in responding to the recession and financial crisis, could demoralize his members. The risk, he said, was a replay of the Democratic blowout in the 1994 elections, when, after the passage of NAFTA and other disappointments to unions, "there was no way to persuade enough working Americans to go to the polls when they couldn't tell the difference between the two parties."
"Now, more than ever, we need the boldness and the clarity we saw in our president during the campaign in 2008," he said.
Trumka stopped short of his September threat that the AFL-CIO might not support the final bill -- after all, he said, labor has been seeking health-care reform for decades. But individual members could sit on their hands. "A bad bill could have that kind of effect," he told reporters. "People could stay home. It could suppress votes."
Organized labor played a crucial role in the 2008 election, turning out members in key states such as Ohio and Pennsylvania where many nonunion, working-class voters resisted Obama. Though Obama has pleased unions on several fronts, he has done little to push labor's biggest priority, the Employee Free Choice Act, which would make it easier for workers to organize.
In 2008, Obama rallied union members' support by repeatedly attacking a proposal by Sen. John McCain (R-Ariz.) to lift the tax exemption for employer-provided health benefits. Now, the White House is strongly supporting the Senate provision to tax benefits above a certain value, $23,000 for a family plan and $8,500 for an individual one.
Supporters argue that such a tax would slow the growth in health-care costs by shifting people into less generous plans, and that it would also lift wages. Opponents note that the tax will fall on many plans that are expensive not because they are lavish "Cadillac plans" but because of an employer's location or the age of its workforce.
Unions prefer the House approach, an income tax surcharge on families earning more than $1 million.
Although firefighting is one "high-risk profession" exempted from the tax, firefighters union head Harold Schaitberger said he was still strongly against it. "It's terrible policy and absolutely disastrous politics," he said. "This is failed promises. We went out and worked hard to deliver our membership [in 2008] . . . . This is a political nightmare for the midterms."
----------
"Economic stimulus has created or saved nearly 2 million jobs, White House says"
By Alec MacGillis, Washington Post Staff Writer; A13; January 13, 2010
The $787 billion economic stimulus package has created or saved between 1.7 million and 2 million jobs, but its impact on the economy ebbed slightly in the final quarter of 2009 compared with prior months, the White House said Tuesday night.
Releasing the administration's second quarterly report to Congress on the stimulus's impact, Christina Romer, chairman of the Council of Economic Advisers, said a third of the tax cuts and spending in the package is out the door. Her office estimates that the stimulus added between 1.5 and 3 percentage points to the growth in gross domestic product in the final quarter of 2009. That estimate, which is in line with other analyses, is lower than her office's estimate of stimulus-related impact in the third quarter, between 3 and 4 percentage points.
Administration officials said often last year that the stimulus's impact would be felt more over time as spending ramped up, but Romer said in a conference call with reporters that the drop-off in GDP impact was not unexpected. The biggest jolt to the GDP came with the first big surge of spending over the summer, she said, and job creation is now following.
"The most important bottom line is to say that close to 2 million jobs have been created or saved by the close of 2009, a truly stunning . . . effect of the act," she said. Still, she added, there is a need for additional spending to spur job creation, as President Obama has called for.
Congressional Republicans have questioned the administration's claims about the stimulus's impact, pointing to the 10 percent unemployment rate nationwide. Romer's new figures are based on macroeconomic estimates, not reports filed by stimulus funding recipients, the next round of which is due later this month.
Separately, the White House has announced a change in the way those reports tally jobs, a response to critics that could make the reports more reliable but make it more difficult to gauge the stimulus's impact over time.
For months, economists and government watchdogs have warned that the job-creation reports should be taken with a heavy grain of salt. The administration deserves praise, they say, for trying to provide transparency in how the $787 billion package is being spent -- whom the money is going to, and for what purpose -- but trying to count the number of jobs created or saved may have been a fool's errand that needlessly undermined the credibility of the overall reporting effort.
This has proven especially true when it comes to "saved" jobs, which the administration says count as much as new jobs, since both keep people off the unemployment rolls. Recipients of stimulus money have used wildly different standards to estimate how many employees would have been laid off if not for the funding -- some have reported every job in their business or agency as "saved," while others have reported zero jobs "saved," even after receiving very large contracts.
The job figures have other shortcomings. Since reporting is required only of the top two layers of funding recipients, the data do not capture jobs created further down the line of suppliers or subcontractors. And stimulus recipients have taken different approaches to counting jobs that are created or saved on a part-time or temporary basis.
To address those concerns, the Office of Management and Budget recently issued new rules for reporting job numbers, aimed at ensuring more consistency. Most notably, the rules instruct recipients unsure how to count "saved" jobs to simply estimate how many employees in a given quarter were working on projects paid for by stimulus dollars, regardless of whether they would have been laid off otherwise.
But there is a downside: The shift in rules means that the numbers reported for the last quarter of 2009 and for the remainder of the stimulus cannot be compared with the job numbers from earlier in 2009. Going forward, recipients will no longer be expected to report a total count of jobs created or saved over time, but simply how many jobs were created or saved in a given quarter.
John Irons of the left-leaning Economic Policy Institute called the new rules a "huge improvement," saying that greater consistency among recipients is more important than having a cumulative jobs count. Even under the old rules, such a tally was going to be unreliable, he said, given the difficulty of counting jobs that only last a month or two.
"This is a better way to do it," he said. "You lose consistency between [the last two quarters] but you gain a whole lot of consistency across agencies. . . . It's a cleaner way to do things."
----------
"White House to issue progress report on anniversary of economic stimulus"
By Alec MacGillis, Washington Post Staff Writer; A11, February 17, 2010
The White House is releasing its first annual report on the American Recovery and Reinvestment Act on Wednesday, summarizing its progress on the first anniversary of President Obama's signing of the massive, politically contentious economic stimulus package.
The $787 billion bill was a classic rendering of the precepts of economist John Maynard Keynes: With employers laying off workers, credit drying up and consumers battening down, the theory went, the government needed to do all it could to inject demand.
But even with most economists agreeing on the need for the stimulus, the package was politically fraught from the outset. Republicans charged the White House with letting congressional Democrats lard up the bill with pet priorities, although the bill's emphasis on education, energy and health care mostly reflected Obama's long-term agenda.
Liberals argued that the package was not big enough, especially given that $70 billion went toward a temporary patch for the alternative minimum tax, which was not seen as a stimulus to the economy.
The White House has acknowledged that its economists argued for a bigger package, but it maintains that the bill passed was the most politically feasible one. The measure got no Republican votes in the House and squeezed through the Senate with three GOP votes.
The stimulus has since become more controversial among the American public. Independent arbiters such as the Congressional Budget Office agree that it helped end the recession and added several percentage points to GDP growth, and that it created or saved at least 2 million jobs.
But with job losses far deeper in 2009 than the administration expected, the stimulus has not kept unemployment from climbing to 10 percent. Republicans have seized on job-creation tallies reported by stimulus recipients, questioning their reliability.
At the same time, Republicans who voted against the bill, as well as Democrats, have touted stimulus spending in their districts.
The package was divided into three main categories:
-- Tax cuts (including $800 for both 2009 and 2010 for most families).
-- Payments, including fiscal aid to states and expanded safety net assistance (such as unemployment benefits, COBRA subsidies and food stamps).
-- Investments in, for example, public infrastructure, energy efficiency upgrades and broadband access.
While much of the investment spending has been slow to ramp up, administration officials say the initiative is on track, with 70 percent scheduled to be spent by October. With most of the state aid and safety net benefits already out the door, the spending will now shift more toward investment projects.
----------
"'Cadillac tax' on health plans would hit union and nonunion jobs equally"
By Alec MacGillis, Washington Post Staff Writer; A13; February 22, 2010
It happens often in Washington: A perception emerges and soon hardens into fact. Take the proposed tax on high-cost insurance plans in the Senate's health-care legislation. Because organized labor took the lead in opposing the tax, the assumption took hold that it would hit unions the hardest.
Both sides made use of this perception. Opponents of the tax could argue that it would hurt a lot of hardworking factory workers or teachers who had traded wage gains in return for good health benefits. Proponents of the tax portrayed opposition to it largely as a special-interest issue driven by self-protective unions.
But according to a new analysis, the conventional wisdom about the tax is wrong: The tax would actually fall equally on nonunion plans. At least 80 percent of the workers whose plans would be subject to the tax in 2019 would be in nonunion jobs, according to the analysis by Ken Jacobs of the University of California at Berkeley Labor Center and William H. Dow, a professor of health economics at Berkeley who was a member of President George W. Bush's Council of Economic Advisers.
This impact is roughly in line with the overall breakdown of nonunion vs. union workers with employer-provided plans. And it would be true under both the version of the tax passed by the Senate and a more labor-friendly one the White House agreed to last month.
The excise tax on "Cadillac" health plans has emerged as one of the most contentious elements of the proposal that congressional Democrats are cobbling together from bills passed by the House and Senate. The tax will probably be included in the health-care proposal the White House is expected to release Monday in advance of the health-care summit President Obama has called.
The bill passed by the Senate would raise $150 billion over 10 years by taxing plans worth more than $23,000 for families and $8,500 for individuals. Any value that exceeds those thresholds would be taxed at 40 percent. Proponents say the tax would slow the growth in health-care costs, as employers and employees shift to less generous plans to avoid it. The savings from switching to lower-cost plans, proponents say, would go into higher wages.
Opponents of the tax, including many House Democrats, doubt that it would slow the growth in costs, arguing that consumers have a limited role in driving health-care spending. They also point to research suggesting that the tax would hit not only lavish plans but also those that are costly because they are in expensive regions or in businesses that have many older workers. And they warn about the political risk of taxing middle-class voters' health benefits, noting that Sen. Scott Brown (R-Mass.) made hay of the tax in his campaign.
The House bill instead relies on a surtax on the wealthy. But Obama has made plain his preference for the tax on high-cost plans. To mitigate its impact, the White House and union leaders last month negotiated revisions, including slightly raising the tax threshold, limiting the tax for businesses with many female or older workers, and exempting government workers and union plans until 2018.
Congressional Republicans have attacked the deal as a carve-out for labor, but according to the analysis, the revisions would also benefit many nonunion workers. The authors, whose work was funded by the California Endowment and the liberal Institute for America's Future, estimate that the revisions would reduce the tax's revenue by $41 billion, of which 71 percent would accrue to nonunion workers.
If employers remained with their current plans, the researchers estimate that 23 percent of plans would be subject to the tax by 2019 in the Senate version, while 14 percent of plans would be hit under the revised deal.
The fate of the tax in the Democratic discussions is unclear. If the labor-friendly revisions are jettisoned, there will be a call to find other ways to minimize the impact on middle-class families.
Rep. Joe Courtney (D-Conn.), a leading opponent of the tax, said the analysis "confirmed what I've been saying all along -- this is a much bigger issue than labor-union households."
"The momentum in the House against it has gotten even worse," he said. "The more this thing has sunk in, it's become politically dangerous in the minds of a lot of members."
----------
"Obama administration plans to close International Labor Comparisons office"
By Alec MacGillis, Washington Post Staff Writer; A15; March 3, 2010
Like a scorekeeper for the world, a tiny unit within the Bureau of Labor Statistics tracks globalization's winners and losers, and the results are not always pretty for the United States. Manufacturing jobs here, for example, have fallen faster since 1979 than in Canada, Germany or Japan. Compensation for those jobs dropped here in 2008 but jumped in South Korea and Australia.
Soon, however, Americans may be spared the demoralization in these numbers: The White House wants to shutter the unit that produces them.
President Obama's budget would eliminate the International Labor Comparisons office and transfer its 16 economists to expand the bureau's work tracking inflation and occupational trends. The White House says the cut, estimated to save $2 million, is one of many difficult decisions the president was forced to make to control spending.
"This budget had to make some tough choices and prioritize the nation's most pressing needs during a challenging economic and fiscal climate," said Office of Management and Budget spokesman Tom Gavin. But the proposed cut has triggered an outcry from an eclectic group of academics, business leaders and union officials -- a reminder that, in the sprawl of the federal government, some seemingly obscure offices have built a loyal following around their discrete missions.
The defenders argue that, given the need to succeed in a global economy, it makes little sense to shut down the office that measures how the country stacks up. There are other sources of foreign data, such as the Organization for Economic Cooperation and Development and the International Labor Organization, but none does as much as the BLS unit to vet and adjust numbers for apple-to-apple comparisons on productivity, unemployment and wage levels, supporters say.
"If you were going to cut this five years after they implemented it 50 years ago, that would be one thing -- who cared then about what's going on in Asia?" said Georgetown University economist Robert Bednarzik, who spent 10 years at the BLS and has started a petition drive to save the unit. "But they've picked the worst possible time to try and get rid of it -- when we're all in this together."
The International Labor Comparisons office dates to the 1960s, when President John F. Kennedy demanded to know whether Western European countries, which were reporting remarkably low unemployment rates, were using a different standard of accounting. The office later expanded to include Asia's emerging economies.
The biggest challenge was China, where reliable statistics are particularly hard to come by. But in 2004, the office contracted with Judith Banister, a former Census Bureau demographer then living in Beijing, who dug up statistical books in local bookstores that helped produce solid data on the Chinese economy. The unit added Brazil to the mix, and in the near future it plans to release its first reports on India.
Banister, a freelance researcher, said U.S. manufacturers need to know what they are up against overseas -- and, in some cases, whether to move work offshore.
Skeptics of free-trade policies criticize the closure for other reasons -- the unit's data, they argue, show just how harsh globalization is for the American worker, a reality that may be inconvenient for an administration generally more trade-oriented than the populist rhetoric of Obama's campaign suggested. They question if the unit is being closed solely for the budget savings, noting that $2 million is a relative pittance, less than 1 percent of the BLS budget.
"The type of documentation [the unit] is putting out could be detrimental to their efforts" on trade, said John Russo of the Center for Working-Class Studies at Youngstown State University.
Gavin, the OMB spokesman, denied that motivation, saying the closure "wasn't a reflection of the quality of the work or a reflection of its usefulness so much as a reflection of priorities."
The budget proposal says the unit's statistics are "not widely used." But supporters point out that the unit's Web site got 1.5 million page views in 2009 -- about 4,000 a day.
Congress could yet decide to retain the program. Sen. Sherrod Brown (D-Ohio), for one, is concerned about the closure, said his spokeswoman Meghan Dubyak. "He plans on working with the administration and [congressional] leadership to ensure that we still have data to address offshoring and competitiveness issues," she said.
Meanwhile, the unit's close-knit group of workers is waiting to learn their fate. Its director, Connie Sorrentino, who has worked in the unit since the 1960s, said her colleagues were "devastated" when they heard the news but have since been heartened by their supporters.
"What helps us keep our chins up are the people who don't want to see it go under," she said. "You find out who your friends are when you're on the chopping block. Though that's a heck of a way to do a customer survey."
----------
The Washington Post, Live Discussion - Online Forum - Q&A, March 23, 2010
What is in the health-care [reform] bill, and how it affects insurers, hospitals and consumers.
About the host: Alec MacGillis covers government and national politics for The Washington Post.
Alec MacGillis writes: "Hello everyone, and thanks for joining us today. I'm here to take any questions about the health care bill's impact, from the impact on the health care industry, which I wrote about in today's paper, to the impact on consumers. Fire away!"
Q. "Income Caps"
Income being a number that's in the eyes of the beholder, what exactly do the caps refer to? Which line on one's tax 1040? total income? AGI? Is the anti-trust exemption in or out and what if any effect on consumers?
A. Alec MacGillis writes:
"The income definitions in the bill are based on adjusted gross income, or perhaps a slightly modified version of it. There is no language on the anti-trust exemption in the bill -- the House has separately passed a bill ending the exemption, but its fate in the Senate is unclear. And some health care experts actually aren't sure that ending the exemption would have as much impact on encouraging competition as would other elements of the bill, such as the creation of the new regulated insurance marketplace, or "exchange," where people without employer-based coverage will buy plans for themselves."
Q. "Insurance Premiums"
How much do you think we can expect our premiums to rise next year? That seems to be the only option for the insurance companies with the additional rules that are being levied on them.... 50% or more wouldn't surprise me at all.
A. Alec MacGillis writes:
"It is quite possible that insurers will keep rising rates in the next couple years in response to the new requirements they will face, but there are some measures in the bill that could actually push the other way, limiting the increases.
"For one thing, starting next year insurers will have to disclose just how much of the money they take in in premium dollars is spent out for medical claims as opposed to being used for profit or overhead. And they will have to spend at least 80 percent of the premium dollar on medical claims in the individual insurance market, and 85 percent of it in the employer-based insurance market.
"Those ratios are higher than what some insurers spend now on medical claims, so that could limit rate increases somewhat. Then there is the basic fact of competition -- while many markets today have very few insurers in them, the whole idea of the new 'exchange' that will start in 2014 is that there will be many more insurers competing for customers. If insurers come into that market with rates that are exorbitantly high, they may lose out to lower-priced competitors. But no one can know for sure what will happen. One thing to keep in mind: most of the insurance regulations in the bill have to do with the individual and "small group" insurance market.
"If there is volatility in rates in the next few years, it will likely be focused there. Employer-based premiums are expected to increase by roughly the same pace as they have been, at least for now, before some of the more systemic attempts to restrain health care spending kick in."
Q. "Insurance for young adults"
My 27-year-old son moved back into my house. He attends college full time and works part time. I can't add him to my health insurance (from my employer) because of his age. Does this bill do anything to help him afford insurance this year? I've read that some provisions don't take effect until 2014.
A. Alec MacGillis writes:
"You're right -- most of the big provisions do not kick in until 2014. At that point, if he still does not have employer-based coverage, he will be able to go to the new 'exchange' and buy a plan there with the help of subsidies based on his income. There are provisions that go into effect before then but none of them will likely bear directly on his situation. Why is it taking so long for the main provisions to kick in? Well, it takes a while to set up the new exchanges. But also, by delaying the biggest costs of the bill, the Democrats were able to shrink the 10-year price tag. If the subsidies had kicked in sooner, the bill would have cost more than $1 trillion over the first 10 years, the magic number they were trying to stay below."
Q. "Dependent children remaining on parent's policies"
Concerning the new requirement that health insurance policies allow dependent children to remain on parent's policies until they are 26, does that apply to dependents who have already been dropped because of their age?
For example, would a 23-year old who had been forced off a policy now be allowed to get back on their parent's policy? I'm a retired federal employee and wondering how this will affect the Federal Employee Health Benefit Program.
A. Alec MacGillis writes:
"To you first question: I am quite sure that dependents who have been dropped because of their age will be allowed to get back on their parents' plan until age 26. (And this is one provision that kicks in this year.)
"The Federal Employee Health Benefit Program will remain mostly unaffected for now. If some of the systemic reforms in the bill actually work, then the FEHBP premiums may increase at a slightly slower rate than they have been (they went up about 8 percent on average last year, I believe.) If the plans' premiums continue to increase at a fast clip, though, the more generous of the FEHBP plans could be subject to the new tax that will go into effect in 2018 on high-priced plans (those worth more than $27,500 for a family plan.) Presumably, the government will do everything it can between now and then to keep the value of the plans from going above that threshold -- that may mean shifting to somewhat higher deductibles and co-pays."
Q. "Penalty for Not Getting Insurance"
The penalty will likely be less than the cost of getting health insurance so what is the incentive for someone young and healthy to get insurance ?
A. Alec MacGillis writes:
"This is one of the biggest challenges looming for the new law. Its success depends to a great extent on how many young and healthy people can be brought into the insurance pool to balance out the older and sicker people who insurers will be required to cover. The insurers argued for a bigger penalty to make sure people got coverage, but the bill's authors worried about the political fallout from a big penalty. The hope is that the bill and the mandate will create a sort of cultural expectation that people get covered -- Massachusetts, for one, has managed to get most people to observe its mandate despite a penalty that at the outset was also quite small (though it's now up around $1,000.) They accomplished that through a very aggressive public education/propaganda campaign (even the Red Sox got involved!) But then again, that was Massachusetts, a liberal state with relatively few uninsured. Whether people in Texas or Colorado will follow suit remains to be seen. One final thought: while there are plenty of 'young invincibles' out there who will pay the penalty instead of getting coverage, we should keep in mind that there are also plenty of young people who have been uninsured not because they don't think they need it but because they couldn't afford it. So they go ahead and buy it."
Q. "How the bill affects me"
I keep my current insurance. I get to pay more taxes. Excuse me for being less than thrilled.
A. Alec MacGillis writes:
"I don't know your exact situation but I wouldn't be so sure that you're paying more taxes under this bill. Is your insurance plan a very high-end one that is worth more than $27,500, the level at which plans will be taxed, and not until 2018 -- only a tiny percentage of plans are now above that value. Do you earn more than $250,000? If so, you'll be paying higher Medicare payroll taxes and a new tax on your investment income. But if you're income is below that, you're not paying any new taxes on this. Sure, the costs of this bill may, down the line, force the raising of taxes more broadly if the numbers in the bill don't work out as planned. But for now, the impact on your wallet may be minimal."
Q. "Unemployed"
After being downsized two years ago, I have been unable to find employment since. My age is a factor. Will I be required to pay an insurance firm monthly premiums even though I have no income, and am depleting my savings?
A. Alec MacGillis writes:
"You will be required to buy insurance starting in 2014 and you will receive subsidies based on your income to help you do so. If you're income is very low, you will be paying a very low share of your income for your premiums. (You may even qualify for Medicaid, which is being expanded up to everyone at 133 percent of the poverty level, or about $29,000 for a family.) BUT...if you truly cannot afford to buy insurance even with the subsidies, you will be granted a 'hardship exemption.'"
Q. "Austin, TX"
Good morning, Alec. My question is one from the consumer point of view. I currently receive partially funded insurance through a large private employer. I've watched over the years as both the costs to my company and my paycheck deductions have risen while at the same time my copays have risen for both doctor visits and prescription medication. While I understand that I may not be directly affected by this legislation, what is the likely effect that HCR will have on the costs of insurance to myself and to my employer, and how soon will any changes start to show?
A. Alec MacGillis writes:
"This is the position that the vast majority of people find themselves in -- with employer based coverage, in plans where premiums and out of pocket costs have been increasing. The bill will not have a direct, immediate impact on you -- it's main target really is the uninsured, small businesses and the people who have to buy insurance in the wild west of today's individual insurance market. But, if the more systemic reforms in the bill work -- getting hospitals and doctors to practice more cost-effective care, making sure people get care when they need it instead of waiting til their conditions worsen -- then the hope is that the growth of health care costs, and of even employer-based premiums, will slow over time."
Q. "Individual vs Company"
My husband and I both have pre-existing health conditions and currently have no health insurance. He owns a small company which employs under 20 people (both full and part-time).
Do you think it would be better for us to get health insurance under my husband's company or should we look around for an individual policy. If I understand the new policy correctly, uninsured, pre-existing people will be in the immediate health care reform (not the "five-years out" class). Did I read this one right?
A. Alec MacGillis writes:
"You may want to explore getting insurance through his company because there is going to be a new tax credit available to help small business buy health plans, starting this year. For individuals with pre-existing conditions, the help is actually not as immediate as many would like -- insurers are not required to sell you policies until 2014, when the mandate goes into effect (because if they had to insure more costly people before the healthy people come into the pool, their business model would collapse.) It's only kids with preexisting conditions that are required to be covered starting now. The one interim provision now for people with preexisting conditions is the creation of a new federal high-risk pool. But I'm not sure what the rules are for who will be eligible for it, and how much the premiums for it will cost. Some experts worry that this pool is not designed or funded as well as it needs to be to be successful. And in any case it will be only temporary, before the main provisions hit in 2014."
Q. "Vulnerably insured"
I've heard a lot of talk of the uninsured and even the underinsured, but no one mentions the vulnerably insured.
My husband and I are starting a business and have individually purchased health insurance. We were left terrified when our previously healthy 5-year-old daughter had H1N1, then pneumonia, then bronchitis.
We were scared to lose our insurance and did not bring her to a pediatric pulmonologist. We're still frightened that our insurance will skyrocket next year even though she's mostly recovered (we hope).
I think folks like us go unmentioned. I am thrilled with the reform, though I know it's not perfect. We shouldn't be forced to choose between our daughter's health and our family's health insurance.
A. Alec MacGillis writes:
"This is a very important point. While most people think the bill has been mainly about covering the uninsured, it applies just as much to people who today have coverage in the individual insurance market, where the rules vary widely from state to state, and where, in many states, people all too frequently see their coverage revoked or payment denied in situations like the one you describe here. Starting this year, insurers in the individual market will have to cover kids with preexisting conditions. And starting this year, they will not be able to revoke coverage once people get sick by claiming to have discovered flaws in people's initial applications -- so called 'rescissions.'"
Q. "Lifetime limits"
Are lifetime limits on insurance coverage banned starting in six months, or starting in 2014? I've seen conflicting info on this.
A. Alec MacGillis writes:
"Lifetime limits are banned this year. Additional rules regarding annual caps on benefits go into effect in '14."
Q. "Public option?"
I'm pleased that progress has been made on this issue, but as a self-employed person, I'm still left paying huge premiums for not-very-good coverage. Is there any hope left for a public option?
A. Alec MacGillis writes:
"It's quite possible that the push for the public option will revive if rates in the new exchange continue to rise sharply. But keep in mind -- as a self-employed person you will be getting subsidies to help you buy coverage, assuming your family income is $88,000 or below. And even if it's above that, you will have more of a choice of plans in the exchange than you do now."
Q. "San Francisco, CA"
Hello, I am a grad student with a pre-existing condition (ulcerative colitis) that makes it too expensive to get private insurance. I currently get insurance through a part time job (make about $8k/year), but I'd like to quit so I can focus on classes more.
What immediate effects will this bill have to make insurance more affordable for me, and what will change with my student loans. In other words, how much free money can I expect?
A. Alec MacGillis writes:
"You may qualify for the new federal high-risk pool that is being created as an interim measure. In 2014, you will get subsidies to help you buy individual coverage and insurers will have to take you on even with your condition. Your student loans will likely see little impact from the new student loan law -- rates will remain unchanged for most people. There will be more money avialable for people who qualify for Pell grants."
Q. "Small Business Impact"
Can someone detail how the various impacts of this bill hit small businesses- tax credits, penalties for not covering employees, sizes of business affected, which businesses can buy into exchanges, etc?
Lots of detail, please. Synergistic explanations of how the moving parts affecting a business with 15 employees that pays the median American worker's wage to all staff and makes a hypothetical profit of $150,000 a year would be wonderful. Then, what about $250 k profit and $500k profit? Thanks.
A. Alec MacGillis writes:
"In brief: companies with fewer than 25 employees, where the employees make less than $50k on average, will qualify this year for new tax credits to help them buy coverage. Companies with under 50 employees also will be exempt from the employer mandate to provide coverage. Companies with more than 50 employees will need to provide coverage or pay a $2,000-per-worker fee. And to qualify for meeting the mandate, the coverage will need to be of a certain minimum value to the worker."
Q. "Abortion funding clarification"
I can't be here for the discussion but I'd really appreciate it if you could answer this question. What exactly does the health care bill say about abortion funding? If the answer to this question is too lengthy do you know where one can find it in the bill and read about it?
A. Alec MacGillis writes:
"This is a very complicated part of the law, but here's the basics: insurers on the new 'exchange' will be able to offer plans that include abortion coverage (as most private insurance plans today now do.) But anyone choosing that plan, whether a young woman or a guy or an older woman, will need to write two separate checks for their premiums -- one to cover the bulk of the coverage, and a second tiny one, like $1 a month or so, to cover the abortion part of the plan. This could be very unwieldy and unpopular with customers, and it's possible that insurers as a result will not offer plans with the coverage, which is why abortion rights groups are not at all happy with the final language, even though it was also deemed unacceptable by anti-abortion groups."
Q. "Insurance"
Doesn't this bill really just change the concept of insurance to not be insurance? I can't run my car into a tree, call up my insurance company and claim a preexisting condition on my car. Because there is no way Democrats will let insurance companies charge these people the price they should pay we will all be paying for it. It's a hidden tax.
A. Alec MacGillis writes:
"Car insurance is different than health insurance, and it always has been. People who work for large employers -- most Americans -- have already been paying for their co-workers. Everyone's part of a big pool and pays the same rate. This is an attempt to make the individual insurance market a similar big pool where costs are spread more broadly."
Q. "Medicare and Medicaid payments"
How are the payments by Medicare and Medicaid to physician offices/hospitals going to be affected by this bill? I don't think people realize that the payments that are provided by Medicaid do not even cover the costs of a physician's office staff (let alone the physician) for the time of seeing such patients.
Many physicians consequently do not see Medicaid patients. Yet Medicaid is suppose to be expanded by this bill. Medicare payments themselves have recently been cut back. Patients get upset when their primary care physician only spend 10-15 minutes with them. This will only get worse if no improvement is made by Medicare and Medicaid reimbursements.
A. Alec MacGillis writes:
"You're right, doctors and hospitals say Medicare and Medicaid reimbursement rates are too low. The bill does raise Medicaid payment rates -- whether it's enough to persuade more doctors to keep seeing Medicaid patients, we'll see. It also raises Medicare payment rates for primary care providers, in recognition of the fact that it would be better for the health care system if more people saw primary care providers instead of costly specialists and if primary care docs were paid better, bringing more people into that line of work."
Q. "Price Gouging"
Is the health care bill going to cut down on price gouging by hospitals?
A. Alec MacGillis writes:
"This is the area where the bill arguably could have done a lot more. It focuses mainly on reforming the insurance industry, and to the extent that it addresses the costs on the provider side of the equation, it focuses mainly on finding ways to reduce the utilization of health care, not the actual price charged by providers. This is the argument being made by insurers, who say that it's hard for them to keep premiums in check when hospitals keep raising rates. But then again insurers were opposed (along with hospitals) to one of the provisions that many experts thought would restrain hospital prices: a public option, which would have given the government more leverage to drive provider prices down. This is going to be the next big battle in health care reform, more directly addressing high prices on the provider side."
Q. "Costs"
I saw that eventually companies will no longer be able to charge higher rates based on a person's medical health. While drastic differences should be discouraged, how does it make sense that a healthy person should have the same cost as someone who is continually in the hospital. This sounds unrealistic to the cost structure of providing health care. Just as all drivers are not the same risk, neither are all patients.
A. Alec MacGillis writes:
"See my answer above on this: we're already sharing the costs of coverage between healthy and less healthy people in the employer-based market. That said, insurers in the new exchanges for individual insurance will be able to charge older people more -- but the ratio will be lower than what they now charge in many states. In Texas, for instance, insurers can charge one person 25 times more than another. Under the law, the maximum age ratio is either 5-1 or 3-1 (Senate bill and House bill were different, and I can't remember offhand which prevailed.)"
Q. "But then again, that was Massachusetts"
I heard a MA state senator say the reason that HCR was so successful in MA was because most of the people had policies with non-profit companies. This is not true of many states.
A. Alec MacGillis writes:
"Not really. Massachusetts did have several advantages -- it had many fewer uninsured than most other states even before the law passed, and it had a very strongly regulated state insurance market, so that it wasn't that much of a leap for insurers and regulators to move to the even more regulated world created by the universal coverage law. But the nonprofit status of insurers matters only so much these days -- a lot of the former Blue Cross plans that are nonprofit are raising rates just as much as the ones that become for-profit, and they're also paying the executives similar multi-million dollar salaries."
Q. "Competition"
We had competitive free market fire companies in colonial America. They didn't work. Whole sections of Philadelphia had little fire protection because the companies did not want to offer contracts where the likelyhood of fire was high. So now we have socialized fire departments.
All other indutrialized countries (except Germany) had competitive free market health insurance at one time. None of them could get it to work. Now they all have universal government run systems.
Economists tell us that competition just doesn't work for items you want everyone to have like fire or police protection or roads or...health care. What makes us believe that our system will be an exception to the rule or to history?
A. Alec MacGillis writes:
"This is the argument for single-payer health insurance. But it's worth noting that some European countries actually don't have pure single-payer programs and instead maintain the semblance of a private insurance industry, though one in which insurers are so heavily regulated that they are, in effect, like public utilities. This is the direction we are moving in. Post-2014, our insurance market will remain more independent than those European countries, but if even that proves unable to restrain costs and controversial insurance practices, we may take another step along that spectrum."
Q. "S-CHIP"
With the children's pre-existing condition clause going into affect immediately, I'm just curious if this takes the place of s-chip.
A. Alec MacGillis writes:
"No, S-chip remains in place for now, since it is for a whole swath of low-income children, not just those with preexisting conditions. The ban on denying coverage to kids with preexisting conditions applies to families who now buy coverage for themselves in the individual market."
Q. "Health Care Anger"
Alec, Why are people so angry over this issue? In the last eight years there have been way more important things to be anger about, but this issue seems to evoke some pretty strong emotions. Whats your take on this?
A. Alec MacGillis writes:
"Good question and one that requires far more thought and space than I'll have here. Clearly, the anger goes beyond the bill in question. The fact is, this bill is, in the grand scheme of health care reform, relatively moderate, incremental and market-based. It is based on the plan that Mitt Romney signed in Massachusetts and on ideas that came out of the Heritage Foundation. It more closely resembles what Nixon proposed in the 1970s and moderate Republican senators proposed in the early 1990s than it does the dreams of single-payer believers."
Q. "Bang for the buck"
How are other countries able to get better results as measured by all the bottom line statisitcs at half the cost per person? If we could emulate their programs, we would get better care and SAVE $1.3 TRILLION each and every year.
A. Alec MacGillis writes:
"There's a lot that goes into this difference, but health care reformers point to three main factors: we demand and use more high-priced medical care (we don't spend more days in the hospital, but we get more treatments while we're there); we pay our doctors and hospitals and drug makers and device makers higher prices than in other countries; and we have a private health insurance system that absorbs plenty of money in profit and overhead."
Q. "Premium Hikes"
I'm wondering if Insurance companies will react like the banks did when they realized that new laws would impact their ability to make a profit at the consumer's expense and they used the time before the law went into effect to raise rates on just about everyone... Is there any provision in the bill that protects consumers from that?
A. Alec MacGillis writes:
"I touched on this concern above -- in brief, starting next year insurers will have to show that they are spending more than 80 percent of premiums on actual medical claims. That will make it harder for them to just raise rates willy-nilly."
Q. "Retiree drug benefits subsidies"
As I understand it, the bill eliminates the subsidies to employers for providing drug coverage for retirees. I've read and heard that the GAAP (Generally Accepted Accounting Principles) treatment of this change will cause many employers to eliminate this benefit. Is this true?
A. Alec MacGillis writes:
"This is an important and overlooked issue that I touched on in today's article. You're right. The Medicare drug benefit also extended a subsidy to large employers so that they would keep providing drug coverage to retirees. This bill taxes that subsidy starting in 2013, likely making it less attractive to some employers to keep providing drug coverage to retirees. And for accounting purposes, employers must declare very soon whether they plan to keep providing the coverage and pay the tax, or drop the coverage. If they drop the coverage, their employees will take the Medicare drug benefit instead. It's worth noting that the Medicare drug benefit will be much more appealing an option than it is today since the 'donut hole' in coverage will be phased out in the next few years."
Alec MacGillis writes:
"Well, that's all I have time for today, unfortunately. Thanks for all the good questions and sorry I couldn't get to even more of them. Clearly, there's a great demand for information on all this, so we'll be sure to have another session soon. Join us again then."
----------
"First wave of health-care changes will target insurers with new rules"
By Alec MacGillis, Washington Post Staff Writer, A08; March 23, 2010
In affixing his signature Tuesday to comprehensive health-care legislation, President Obama will set in motion a fundamental shift across a sprawling industry, from insurers who will face an expanding list of restrictions to hospitals and doctors confronted with new incentives to practice more-efficient care.
The law will have a gradual impact on many consumers. In coming months, parents will be able to keep their children on their plans until age 26; people over 65 will get broader coverage from the Medicare drug benefit; and insurers will be barred from revoking coverage when people get sick and refusing to cover children with medical conditions.
The requirement that most everyone carry health insurance will not kick in until 2014, along with subsidies to help people pay for coverage.
But the law's impact will be more profound for the health-care industry in a country where one in six dollars is spent in that sector. Every part of the industry will be affected, with pharmaceutical companies, hospitals and makers of devices subject to new rules, billions of dollars in fees and relinquished reimbursements in return for the business growth that expanded coverage will bring.
By far, the most direct effect will be on insurers. Over the next several years, health insurance will evolve into something more closely resembling a publicly regulated utility: It will have a guaranteed base of customers, thanks to the coverage requirement, but it will be bound by much tighter restraints than today's individual insurance market, where regulations vary widely from state to state.
"This legislative force is significant," said David Cordani, chief executive of Cigna, a major insurer. "It will drive, over the next couple decades, unprecedented changes, all of which aren't really understood yet."
Starting this year, insurers will no longer be able to cap lifetime benefits, which will scramble the actuarial formulas many insurers use and potentially lead them to raise prices for individual policies. But their ability to raise rates sharply for individual insurance plans will be limited by a rule, to take effect next year, requiring insurers in the individual market to spend 80 cents of every premium dollar on claims, a higher "medical loss" ratio than many now adopt.
Some worry that there will be little to keep insurers from driving up their insurance rates for individual policies, which people without employer-based coverage can purchase on a new state-run "exchange" starting in 2014. Liberals argued unsuccessfully for a government-run plan, or "public option," to guard against such rate increases, and Obama proposed a new federal rate-oversight authority, but congressional rules kept it from being included in the final package.
But industry analysts predict that rate increases will be held in check somewhat by the new rules on medical loss ratios and by heightened competition for customers, who will have more choice of plans than they currently do in the individual market. "They're free to price themselves into oblivion if they choose to do so," said Sheryl Skolnick, an industry analyst with CRT Capital Group.
Taking a particularly big hit to their business model would be insurers who rely heavily on selling Medicare Advantage policies. The legislation sharply reduces federal subsidies for those plans, which analysts say will probably lead many smaller insurers to stop offering them.
Overall, industry analysts say that the growth in customers could come close to balancing the cost of the new regulations for insurers, with smaller profit margins on a broader base of business. Ana Gupte, an analyst with Sanford Bernstein, said insurance stocks held up Monday because most of the negative impact of the legislation had been priced in long ago. Insurers "come out a net negative, but not severely net negative," she said.
The impact on hospitals and doctors will be less immediate. Industry groups for medical providers agreed to several hundred billion dollars in reductions in Medicare and Medicaid reimbursements to help pay for the overhaul, on the theory that expanding coverage would mean that more patients would be paying for the care they get.
The cuts will be not be easy to absorb, but hospitals will have several years to prepare, said Thomas P. Glynn, chief operating officer for the Partners HealthCare hospital network in Massachusetts, where a universal coverage law was approved in 2006. "At least it was done in a way where we can know what it is upfront and can start managing against it," he said.
The legislation headed to Obama has an array of pilot programs and incentives for providers to work more cost-effectively, including basing Medicare payments on a patient's condition instead of on the number of procedures. But overall, analysts say, it will probably be a boon for most hospitals and doctors, because it will make it less likely that they will be faced with patients who cannot pay and show up too late for treatment.
"You don't pour nearly a trillion dollars into the health-care space without some of the money flowing down into the hospital system and other providers," said Skolnick, the analyst. "There will be more people getting care from the right channels at the right time, and more of the care will be compensated."
Some experts say a shortcoming in the legislation is that it does not have a deeper impact on medical providers. They predict that the government will have to take more action later to restrain the growth in health-care costs by holding down the prices charged by providers, whether through a public option or rate-setting.
But the new system at least creates more of an incentive for future cost control: Now that the government will be subsidizing people's coverage, it will have more of a stake in keeping medical costs in check.
"In terms of the way providers are affected, it's probably not as big a change as it should have been," said John Holahan of the Urban Institute. "But you have the structure to deal with that in place, going forward. . . . If premiums continue to skyrocket, even with subsidies, insurance will be deemed unaffordable, and the whole thing will unravel."
Although much of the attention has focused on the health-care industry, the law also will carry an immediate impact for many employers. Businesses with fewer than 25 employees will start receiving tax credits to help them buy coverage, and large employers who pay for retirees' drug coverage must immediately declare, for accounting purposes, whether they intend to keep the coverage. The other option would be to send their retirees into Medicare's drug benefit program by 2013, when the government cuts the subsidy employers receive to offer their coverage.
----------
April 13, 2020
When I was a teenager growing up in Pittsfield, my brother and me volunteered to cleanup the streets, parks, and river banks in Pittsfield (Mass.) I am nearly 45 years old now, but back in my youth, we took a lot of pride in Pittsfield. I saw a newly painted house this past weekend while walking with my family in our new town of Amherst, NH, that was painted purple with white trim. I said to my brother it was the colors from Pittsfield High School. My mom said to us that when we were teenagers, we took a lot of pride in our home under the dome. My brother graduated from PHS in 1992 with an incredible class that includes Hollywood movie star Elizabeth (Mitchell) Banks, Washington Post journalist Alec MacGillis, and Kim Cobb, who is a paleoclimatologist and oceanographer who testified with Gov. Charlie Baker at a U.S. House Committee on Natural Resources hearing on climate change in early-February of 2019. Alec MacGillis and Kim Cobb both graduated from Yale University. I graduated from PHS the next year in 1993, but I tell my brother that I am in awe of the achievements of his incredible PHS class.
- Jonathan Melle
----------













































































































































.png)
















































































































































































































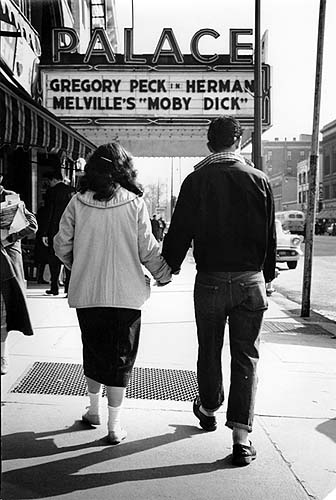







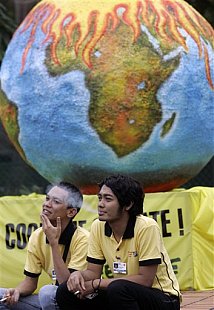




































No comments:
Post a Comment